Why Nurse-Guided Care Matters: Clinical Oversight for Safer, Personalized Home Care in Philadelphia

At its core, nurse-guided care centers registered nurses as the clinical decision-makers for in-home care—bringing medical judgment, safety checks, and individualized plans directly into Philadelphia homes. Below we walk through how RN clinical oversight works in a home setting, why it lowers complications and readmissions, and how caregivers and families gain confidence through focused education and timely clinical intervention. You’ll get a clear view of the day-to-day workflow—from assessment to RN-led care planning and coordination—and see how specialized pathways for dementia, post-surgical recovery, and chronic disease management look in practice. We also cover technology tools such as virtual assessments and remote monitoring that help RNs respond faster and fine-tune care plans. Finally, we outline the cost-effectiveness drivers that often make nurse-guided models more efficient than institutional alternatives. Throughout, we reference practical search terms like nurse guided care Philadelphia, clinical home care PA, and RN supervised home care so families and clinicians can find relevant local resources.
What Is Nurse-Guided Home Care and How Does It Work in Philadelphia?
Nurse-guided home care is a clinical model where a registered nurse leads the initial evaluation, designs and updates the care plan, and oversees clinical tasks to prevent setbacks and help recovery. It depends on RN clinical judgment, routine monitoring, medication reconciliation, and active coordination with doctors and therapists to keep care timely and appropriate. In Philadelphia’s mixed healthcare landscape—where people often move between hospitals, clinics, and home—this approach reduces gaps by giving families a single clinically accountable point of oversight. The sections that follow describe typical RN activities, how they differ from non-clinical home support, and what families and clinicians should look for when clinical needs are present.
What Does Clinical Oversight by Registered Nurses Involve?

Clinical oversight starts with a full assessment of medical history, current medications, functional ability, and home safety risks to set a reliable baseline. RNs use structured tools to spot early signs of decline, perform medication reconciliation to prevent errors, and establish clear clinical goals with measurable milestones for recovery or chronic disease control. Ongoing monitoring can include daily or weekly checks, trending vital signs, wound reviews, and regular updates with prescribing clinicians so care escalates quickly when needed. Nurses also teach and supervise caregivers on task-specific skills, ensuring delegated duties meet clinical standards and that caregivers know exactly when to contact the RN or physician.
How Does Nurse-Guided Care Differ from Traditional Home Care?
The main differences are scope, accountability, and expected clinical results. Traditional home care typically focuses on daily living assistance—bathing, meals, companionship—while nurse-guided care adds skilled clinical management: medication oversight, clinical monitoring, wound care, and care coordination. Because an RN serves as the clinical leader, accountability and the ability to interpret clinical data, adjust plans, and coordinate with hospitals or specialists are higher. That clinical focus usually produces stronger measurable outcomes—fewer ER visits, better symptom control, and fewer preventable complications—than non-clinical assistance alone.
What Are the Key Benefits of Nurse-Led Home Care in Philadelphia?

Nurse-led home care pairs clinical expertise with individualized, in-home interventions that prevent decline and support recovery. Core mechanisms include proactive monitoring, thorough medication reconciliation, and rapid clinical response to early warning signs—steps that stop small issues from becoming emergencies. This model also respects quality-of-life goals by aligning care plans with patient preferences and family needs, and it boosts adherence through caregiver training and ongoing coaching. Below we summarize the main benefits and explain how each one produces better results for patients and families.
Nurse-led home care delivers three foundational benefits:
- Reduced Hospital Readmissions: Continuous RN monitoring and medication reconciliation address common causes of readmission before escalation occurs.
- Improved Clinical Outcomes: Focused interventions—wound care, symptom control, medication adjustments—help manage chronic conditions and speed recovery.
- Stronger Family Support: Education and care coaching ease caregiver uncertainty and improve adherence to treatment plans.
Together, these benefits create a clinical safety net that makes home care safer and more personalized for Philadelphia families.
Intro to benefit mechanisms table and how mechanisms map to outcomes:

This table shows how specific RN activities link directly to measurable outcomes, helping explain why nurse-guided care improves safety and lightens system strain.
To see this in practice, Home Matters Caregiving applies a nurse-guided model in Philadelphia that centers a clinical leadership team, thorough family education, nurse-led caregiver training, virtual assessment tools, one-on-one personalized care, and senior care coaching. These operational elements show how the benefits above translate into predictable, reliable services families can expect from an RN-supervised program.
How Does Nurse-Guided Care Prevent Hospital Readmissions?
Nurse-guided care lowers readmissions by closing the common transitional gaps: medication errors, unresolved symptoms, and missed follow-up. RNs perform medication reconciliation at discharge, confirm patient and family understanding, and set up early follow-up monitoring to check adherence and spot side effects. Symptom-monitoring protocols and early-warning criteria give nurses clear thresholds for escalation so problems are addressed before hospitalization becomes necessary. Evidence and program data consistently show that structured RN follow-up and fast clinical responses are linked to reduced 30-day readmission rates—particularly for conditions like heart failure and in post-operative recovery.
Nurse-Led Heart Failure Education for Elderly Patients
This pilot study evaluates a nurse-led, patient-centered education program for older adults with heart failure, testing whether focused nursing education improves knowledge, self-efficacy, and self-care behaviors—and ultimately health outcomes.
Pilot testing of the effectiveness of nurse-guided, patient-centered heart failure education for older adults, 2018
Specific prevention mechanisms include:
- Medication reconciliation and adherence checks by RNs within 48–72 hours of discharge.
- Symptom-monitoring protocols with clear escalation thresholds.
- Timely coordination of outpatient therapies and physician follow-up appointments.
These measures work together to close gaps in transitional care and reduce the chance that a preventable complication leads to rehospitalization.
In What Ways Does Nurse-Led Care Improve Patient Outcomes and Quality of Life?
Nurse-led care improves outcomes by tying interventions to measurable goals and using ongoing assessment to fine-tune treatment. RNs follow evidence-based protocols—wound care standards, symptom-management algorithms, and medication guidelines—to lower complication rates and support functional recovery. Beyond clinical measures, nurse-guided care also supports emotional well-being through consistent communication, dignity-preserving practices, and personalized goal setting that keeps care centered on what matters to the person. Common results include better symptom control, fewer emergency visits, and improved functional status when RN oversight is consistent.
Key outcome improvements include enhanced symptom control, reduced acute care use, and better patient-reported quality of life—benefits that come from RNs’ ability to synthesize clinical data, anticipate risks, and coordinate multidisciplinary care in the home.
How Does Nurse-Guided Care Support Families and Caregivers in Home Health?
Nurse-guided care eases the burden on families by sharing clinical responsibility, delivering structured education, and offering practical coaching that reduces caregiver stress. RNs train family caregivers on medication administration, safe mobility, and symptom recognition, and provide written care plans plus follow-up coaching to reinforce learning. For comprehensive support and training for caregivers, explore our Caregiver Services. This support reduces the daily time and decision-making load and helps caregivers know when to escalate concerns. The model favors collaborative care planning so families clearly understand who is responsible for each clinical task and when to contact the RN or other clinicians.
What Educational Resources Do Nurses Provide to Families?
Nurses provide focused educational modules tailored to the patient’s condition and the caregiver’s skill level—covering medication management, wound care basics, fall prevention, and emergency response plans. Teaching happens through in-person demonstrations, printed care guides, and virtual coaching sessions that reinforce hands-on skills and clinical reasoning. RNs also instruct families on using monitoring devices and interpreting basic data so they can flag concerning trends early. Multiple learning formats give caregivers reliable references and on-demand support for day-to-day clinical tasks. For additional guides, articles, and support materials, visit our Resources section.
How Does Clinical Oversight Reduce Caregiver Burden?
Clinical oversight lowers caregiver stress by clarifying responsibilities, giving easy access to RN guidance, and organizing care tasks into predictable routines that reduce uncertainty. With an RN supervising clinical duties, families spend less time troubleshooting medication questions or interpreting symptoms on their own, which cuts stress and the number of emergency calls. Scheduled check-ins and clear care plans create dependable touchpoints for questions and decision validation. Over time, this consistent support results in measurable drops in caregiver-reported stress and fewer crisis-driven healthcare visits.
In practice, Home Matters Caregiving emphasizes comprehensive support and nurse-led training for caregivers—showing how an RN-focused model can deliver practical family coaching while keeping clinical safety front and center.
Which Specialized Nurse-Guided Services Are Available in Philadelphia Home Care?
Specialized nurse-guided services in Philadelphia use condition-specific clinical pathways led by RNs to manage complex needs at home. Typical offerings include nurse-guided dementia care, post-surgical transitional nursing, chronic disease management (heart failure, COPD, diabetes), advanced wound care, and telehealth-enabled monitoring. Each service pairs clinical assessment with protocol-driven interventions and caregiver education to form a cohesive plan tailored to the condition’s specific risks. The table below outlines common services, the RN’s role, and expected outcomes.
Introductory table mapping services to RN roles and outcomes:
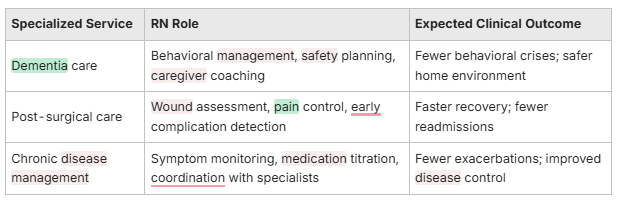
This mapping shows how targeted nurse activity can produce better clinical outcomes, especially when care is individualized and closely supervised.
Specialized service features include:
- Condition-specific clinical protocols with measurable outcome indicators.
- Integrated coordination with physicians and rehabilitation services to support recovery.
- Remote monitoring and virtual assessments to extend RN oversight between visits.
Understanding these features helps families see how nurse-guided care makes complex in-home treatment practical. Home Matters Caregiving delivers these services through a clinical leadership team, nurse-led training, and virtual assessment tools—enabling one-on-one personalization and senior care coaching matched to each person’s needs.
How Is Nurse-Led Dementia and Alzheimer’s Care Delivered?
Nurse-led dementia care centers on behavior management, environmental risk reduction, medication oversight, and caregiver coaching to keep people safe and comfortable. RNs identify triggers for challenging behaviors and use non-drug strategies—like consistent routines and environmental adjustments—to lower agitation and fall risk. Medication regimens are regularly reviewed to avoid interactions or side effects that can worsen cognition, and caregivers receive focused training on de-escalation and safe mobility. This holistic approach reduces crisis admissions and gives caregivers practical strategies supported by clinical backup.
What Role Do Nurses Play in Post-Surgical and Chronic Disease Management?
For post-surgical and chronic disease pathways, RNs perform wound checks, monitor vital signs and symptom progress, and coordinate treatment adjustments with surgeons or specialists as clinical data demand. Nurses follow protocol-driven wound care, apply advanced dressings when needed, manage pain safely, and look for early infection or decompensation signs. For chronic conditions, RNs teach self-management techniques, adjust medications under standing orders or physician guidance, and use remote monitoring to flag concerning trends. These RN-led actions reduce complications and help many patients recover or stay stable at home instead of returning to the hospital.
What Makes Home Matters Caregiving’s Nurse-Guided Model Unique in Philadelphia?
Home Matters Caregiving’s nurse-guided model blends clinical leadership, advanced caregiver training, and virtual assessment tools to deliver accountable, personalized home care for older adults and medically complex clients. Key value points—an experienced clinical leadership team, comprehensive family education, nurse-led caregiver training, smart virtual assessments, one-on-one care, and senior care coaching—are built into daily operations to ensure consistent RN oversight and fast care-plan adjustments. To understand what truly sets us apart, explore Why Home Matters. This model concentrates clinical decision-making with RNs who evaluate risk and coach caregivers, combining hands-on nursing expertise with technology to boost safety and responsiveness in the home.
Who Comprises the Clinical Leadership Team and What Is Their Training Philosophy?
The clinical leadership team usually includes RNs, advanced practice nurses, and a clinical director who set standards, train staff, and run quality assurance to keep care safe and effective. You can learn more about our team and philosophy on our About Us page. Their training philosophy emphasizes competency checks, scenario-based mentorship, and ongoing education to sharpen clinical judgment and task-specific skills. Supervision, regular competency assessments, and shared best practices ensure that caregivers work under RN direction with clear protocols and escalation pathways. That structure helps make clinical decisions consistent and gives caregivers the confidence to perform delegated tasks safely.
How Do Virtual Assessment Tools Enhance Personalized Care Plans?
Virtual assessment tools—secure video visits, remote vitals reporting, and structured telehealth check-ins—give RNs timely clinical data to make faster, more accurate plan adjustments. Remote monitoring reveals trends in vitals and symptoms so nurses can intervene proactively, while virtual visits let RNs observe mobility, medication routines, and wound sites between in-person visits. These tools improve documentation, streamline communication with physicians, and shorten the time needed to change treatments when indicators shift. Integrating virtual assessments into RN workflows increases personalization and responsiveness while maintaining clinical oversight across distance.
Nurse-Led Digital Health Interventions for Symptom Management
Nurse WRITE, an 8‑week web-based, nurse-guided digital health intervention for symptom management in women with recurrent ovarian cancer, offers a model for measuring engagement and effectiveness in provider-guided digital programs.
Measuring engagement in provider-guided digital health interventions with a conceptual and analytical framework using nurse WRITE as an exemplar …, TH Thomas, 2024
How Cost-Effective Is Nurse-Guided Home Care Compared to Institutional Care?
Nurse-guided home care can be more cost-effective than institutional options by preventing avoidable hospital stays, directing resources where they matter most, and aligning services with patient goals to avoid low-value care. Cost advantages come from fewer ED visits, shorter inpatient stays, and targeted therapies that address high-impact needs rather than blanket institutional services. When you factor in long-term outcomes—better chronic disease control and fewer acute exacerbations—the savings from nurse-guided home care often offset higher per-visit RN costs. The table below compares typical settings, their cost drivers, and the longer-term financial or clinical impact.
Introductory cost-effectiveness table:
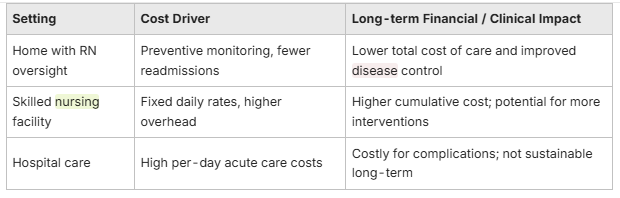
This comparison highlights how targeted RN interventions at home reduce high-cost events and support clinical stability, yielding long-term savings and more patient-centered outcomes.
What Are the Long-Term Savings from Reduced Hospitalizations?
Long-term savings come from fewer readmissions, shorter acute stays, and less dependence on institutional post-acute care—each avoided hospital day represents significant cost avoidance compared with investments in RN oversight. By preventing common readmission causes—medication errors, unmanaged symptoms, or wound problems—nurse-guided programs lower costly utilization. Real-world evaluations show that cutting even a small number of readmissions annually can offset enhanced RN supervision costs across populations with chronic disease. Those savings accumulate over months and years as better disease management reduces acute care needs.
List of long-term financial benefits:
- Reduced emergency department use and fewer inpatient admissions.
- Lower overall expenses for post-acute care through targeted home interventions.
- Delayed or avoided institutionalization by preserving function and safety at home.
Optimizing care to prevent high-cost events delivers both measurable clinical value and financial benefits.
How Does Personalized Nurse Care Optimize Resource Use?
Personalized nurse care conserves resources by directing interventions to where they have the greatest clinical impact and by cutting unnecessary services through RN triage and targeted planning. RNs prioritize medication optimization, high-yield therapies, and timely referrals to prevent downstream inefficiencies like duplicate testing or inappropriate specialist visits. They also coordinate durable medical equipment, therapy services, and caregiver training to ensure interventions are used effectively and not duplicated. This prioritization speeds recovery and reduces overall system cost by focusing on well-chosen clinical actions.
Practical resource-optimization strategies include RN-led triage to limit unnecessary clinician visits, protocol-driven therapy use to ensure correct dosing and timing, and remote monitoring to replace some in-person checks while maintaining safety. Together, these approaches preserve quality care at lower total cost.
- Target high-impact interventions: Prioritize wound care, medication reconciliation, and symptom control.
- Use RN triage to prevent unnecessary escalation: RNs determine when physician involvement is required.
- Leverage technology for efficiency: Remote monitoring reduces visit frequency without compromising safety.
These practices align clinical priorities with resource stewardship to maximize both patient outcomes and financial sustainability.
Frequently Asked Questions
What types of patients benefit most from nurse-guided home care?
Patients with chronic conditions, those recovering from surgery, and people with cognitive impairment such as dementia benefit most from nurse-guided home care. These individuals often need ongoing clinical oversight, medication management, and adaptable care plans. Registered nurses provide the structure and expertise that prevent complications, cut hospital readmissions, and support daily living. Families also gain from education and training that help them manage care confidently at home.
How do virtual assessments work in nurse-guided care?
Virtual assessments use secure video visits, remote vital-sign reporting, and telehealth check-ins to let RNs monitor patients between in-person visits. Nurses review symptoms, observe mobility or wound sites, and adjust care plans as needed—often without requiring a clinic visit. Virtual tools improve communication among patients, families, and medical teams and enable faster responses when conditions change.
What training do caregivers receive in nurse-guided home care?
Caregivers receive hands-on instruction in medication administration, safe transfers and mobility, and early symptom recognition. RNs offer demonstrations, written care plans, and ongoing coaching to reinforce skills. This structured training builds caregiver competence and confidence while clarifying when to contact the RN for clinical guidance.
How does nurse-guided care address medication management?
Medication management begins with a systematic reconciliation—reviewing all prescriptions, supplements, and over-the-counter drugs—so patients and families understand the regimen and potential side effects. RNs perform follow-up checks to confirm adherence and coordinate changes with prescribers when needed. This proactive approach reduces medication errors and improves safety and outcomes.
What role do families play in nurse-guided home care?
Families are key partners: they help shape care plans, participate in training, and provide day-to-day support. RNs collaborate with family members to create practical, person-centered plans that reflect patient preferences. Education and structured support reduce caregiver stress and help families make informed decisions about escalation and care priorities.
How can nurse-guided care improve the quality of life for patients?
Nurse-guided care improves quality of life by combining clinical management with attention to emotional and functional needs. RNs focus on symptom control, rehabilitation goals, and emotional support, and they involve patients and families in decisions. Regular communication and education help people stay engaged in their care, leading to fewer emergencies and greater comfort at hom


