How In-Home Care Helps Philadelphia Seniors Manage Chronic Disease: Practical, Compassionate Support

In-home chronic disease care in Philadelphia means coordinated, non-hospital services delivered where a senior lives. The goal is simple: manage long-term conditions, lower complications, and keep people independent and comfortable at home. This guide shows how
in-home caregivers support common conditions — diabetes, Parkinson’s, heart disease, dementia, and stroke — and offers concrete steps families can use to build safer, more effective care plans. You’ll find the core elements of home-based chronic care — medication management, help with daily activities (ADLs), remote monitoring, and care coordination — plus condition-specific caregiver tasks and local Philadelphia resources. Explore our
additional services to see how we can support your family. Many families struggle with fragmented care, frequent hospital visits, and confusing program navigation; this article gives clear actions, checklists, and comparisons to help caregivers, relatives, and decision-makers choose and oversee in-home support. The content is organized into six practical sections: what in-home chronic care covers, caregiver roles for diabetes and Parkinson’s, measurable benefits of home care, how personalized plans are made and updated, caregiver qualifications in Philadelphia, and local resources families can use.
What Is In-Home Chronic Disease Care for Seniors in Philadelphia?
In-home chronic disease care delivers a mix of services at the senior’s residence to manage ongoing health conditions, prevent emergencies, and preserve everyday function. Care teams provide medication oversight, help with ADLs, vital-sign checks, fall-prevention measures, and regular communication with clinicians to lower readmission risk and support independence. This often includes nurse-guided care for more complex needs. This approach works because it fits medical routines into daily life and gives clinicians ongoing observations that enable earlier intervention. In Philadelphia, effective in-home care coordinates with neighborhood clinics, telehealth, and local community programs to address transportation challenges, seasonal weather issues, and urban resources. Knowing these components helps explain why tailored, home-based care often outperforms episodic clinic visits for managing chronic illness in the city.
How Does In-Home Care Support Seniors With Chronic Illnesses?

In-home care provides everyday, practical support that lowers complications and helps seniors stay functional. Caregivers remind and assist with medication timing, confirm correct doses, and note symptoms for clinicians — actions that cut medication errors and adverse events. They help with ADLs like bathing, dressing, and meal prep to protect nutrition and prevent deconditioning, and they recommend mobility strategies and simple home modifications to reduce falls. These personal and companion care services are vital for daily well-being. Caregivers can also set up remote-monitoring devices or manage telehealth visits so clinicians can act on abnormal readings quickly, reducing unnecessary emergency-room trips. Combining hands-on help with proactive monitoring creates a stable, predictable environment that supports long-term disease management and improves daily life.
Which Chronic Diseases Are Common Among Philadelphia Seniors?
Seniors in Philadelphia commonly live with diabetes, Parkinson’s disease, heart disease, dementia, and stroke-related impairments. Each diagnosis needs different in-home supports and monitoring approaches. Diabetes care centers on blood sugar control, nutrition, and foot care to avoid serious complications; Parkinson’s care prioritizes mobility, precise medication timing, and speech/swallow strategies. Heart disease and post-stroke needs focus on medication adherence, pacing activity, and cardiovascular monitoring, while dementia care emphasizes routines, supervision, and behavior strategies to keep someone safe. Knowing which conditions are most likely and what each requires helps families and caregivers prioritize tasks and choose services that will make the biggest difference quickly.
How Do Caregivers Assist Seniors With Diabetes and Parkinson’s Disease at Home?
Caregivers take on distinct but overlapping responsibilities for diabetes and Parkinson’s, targeting the biggest risks for each while supporting daily life. For diabetes, caregivers help maintain medication and insulin schedules, plan meals and timing, assist with glucose checks when needed, perform daily foot inspections, and alert clinicians when readings fall outside targets. For Parkinson’s, caregivers focus on safe transfers, using mobility aids, supporting exercise and balance routines, timing medications to reduce “off” periods, and using safe-mealtime techniques to lower aspiration risk. Both roles depend on careful observation, accurate documentation, and timely communication with healthcare providers to prevent complications and support independence.
Different conditions call for specific caregiver tasks and measurable outcomes. The table below compares typical diabetes and Parkinson’s care tasks with expected results so families can see practical responsibilities at a glance.
Care tasks vary by condition; matching tasks to outcomes helps measure impact.
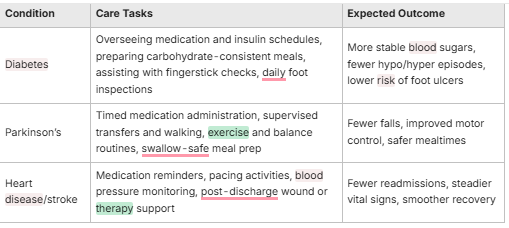
Key Caregiver Roles in Diabetes Management
Caregivers supporting diabetes focus on steady medication use, predictable nutrition, monitoring, and preventive foot care to avoid long-term problems. Day-to-day tasks include confirming medication timing and doses, helping with glucose checks when needed, preparing meals that fit prescribed carbohydrate plans, and inspecting feet for cuts or blisters that could worsen. Our medication assistance ensures adherence and safety. Caregivers record blood sugar trends and notify clinicians about concerning patterns, and they teach family members to spot hypoglycemia and respond in an emergency. These practical steps reduce hospitalization risk and help seniors maintain steady metabolic control, especially when memory or mobility issues make self-care harder.
How Parkinson’s Home Care Improves Daily Living
Home care for Parkinson’s prioritizes mobility support, consistent medication timing, adaptive techniques for daily tasks, and therapy-based routines that protect function and safety. Caregivers assist with transfers and steady walking, help practice balance exercises with therapists, and keep medication schedules tight to limit motor fluctuations. Mealtime strategies and swallow-safe techniques reduce aspiration risk, while cueing and simplified instructions support speech and social engagement. For more specific guidance, explore our home care assistance tips for Parkinson's. These measures together preserve independence and lower the stress families face when managing complex motor and non-motor symptoms.
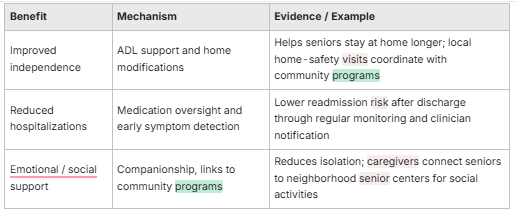
What Are the Benefits of In-Home Care for Seniors Managing Chronic Diseases in Philadelphia?
In-home care offers clear, measurable benefits for seniors with chronic illness: better daily function, fewer hospital visits, and practical emotional and social support tailored to Philadelphia neighborhoods. Key mechanisms include continuous medication oversight, early symptom detection through regular checks, personalized routines that respect preferences, and care coordination that connects seniors to local clinics and telehealth. Those benefits translate to fewer emergency visits, improved symptom control, and higher reported quality of life among seniors receiving skilled home support. In Philadelphia, linking in-home care with neighborhood senior centers and community health programs strengthens outcomes by addressing social and access barriers.
Small community gestures make a real difference, too. Simple acts — consistent companionship, helping with favorite pastimes, or bringing a small comfort — lift mood and improve adherence to care routines. From a local perspective, familiar faces and neighborhood connections are powerful complements to clinical care.
The table below summarizes the main benefits, how they work, and Philadelphia examples that show what results look like locally.
A concise view of how in-home services map to benefits and local examples.
How Does In-Home Care Enhance Quality of Life and Independence?
In-home care preserves routines and lets seniors live safely in familiar surroundings with tailored help for ADLs, mobility, and social engagement. We offer care on your schedule, adapting to individual needs and preferences. Caregivers build individualized schedules that balance medical needs with personal preferences, promoting autonomy and reducing reliance on institutional care. Social activities — friendly conversation, escorted errands, or virtual visits — help prevent loneliness and support adherence to treatment plans. For comprehensive, around-the-clock support, consider live-in care in Philadelphia. We also offer live-in care in West Chester, PA, Phoenixville, PA, and Chester, PA. Together, these supports keep physical function, stimulate cognition through engagement, and give seniors a greater sense of control.
How Does In-Home Care Reduce Hospitalizations and Health Risks?
Prevention, adherence, and early communication are the primary ways in-home care cuts acute events and readmissions. Caregivers track changes in weight, blood pressure, glucose, or wound status and flag trends for clinicians before crises develop. They make sure post-discharge instructions are followed — timed meds, activity limits, and therapy schedules — addressing common causes of readmission. Coordinated plans between primary care, specialists, and the in-home team create a feedback loop where small actions at home prevent larger problems, lowering emergency visits and improving long-term outcomes. We also leverage innovative care options, including remote monitoring, to enhance safety and responsiveness.
How Are Personalized Care Plans Developed for Chronic Disease Management at Home?

Personalized care plans start with a thorough assessment: medical history, current medications, functional status, cognitive screening, social supports, home safety, and the senior’s personal goals. This commitment to 1-on-1 personalized care ensures every aspect of a senior's well-being is addressed. Clinicians, caregivers, family members — and the senior whenever possible — work together to set measurable goals, anticipate risks, and set monitoring frequency. This collaborative approach defines the roles of your care team. The plan lays out daily routines, medication schedules, therapy goals, and clear steps for worsening symptoms. It also defines who communicates with clinicians and how escalations happen, so everyone on the care team knows their role.
Teams use practical checklists to make sure plans are realistic, complete, and adaptable as needs change.
- Initial intake and medical history review to capture diagnoses and medications.
- Functional and cognitive screening to identify ADL/IADL support needs.
- Home safety assessment and plan for modifications to lower fall risk.
- Goal-setting with measurable targets (for example: glucose range, mobility milestones).
- Schedule for monitoring and clinician communication.
These steps create a clear roadmap for care delivery; the next section explains how plans are updated as needs evolve.
Personalized Care Planning for Chronic Condition Management
Personalized Care Planning (PCP) is a collaborative method for managing chronic conditions that emphasizes shared decision-making and joint goal-setting between clinicians and patients. A process evaluation in the PROSPER feasibility trial examined how PCP can be implemented for older adults with frailty in community settings.
What Is the Assessment Process for Creating Tailored Care Plans?
The assessment is a structured review of medical, functional, cognitive, and environmental factors that shape an individualized care plan aligned with clinical goals and personal preferences. Teams perform medication reconciliation, ADL assessments, mobility and fall-risk screens, nutritional checks, and social-support mapping to identify strengths and and risks. Input from primary care and specialists clarifies medical priorities, while family interviews reveal daily routines that support adherence. The end result is a baseline plan with clear monitoring metrics and assigned responsibilities to guide caregivers and clinicians.
How Are Care Plans Adjusted Over Time for Changing Needs?
Care plans change through scheduled reviews and event-driven reassessments after hospital discharge, symptom changes, or new diagnoses, following a documented communication protocol. Regular monitoring — daily logs, weekly trend reviews, or monthly clinician check-ins — helps detect declining function or medication side effects early. When needs shift, teams revise medications, add therapies, modify mobility supports, or increase supervision, and they record those changes so everyone stays aligned. Ongoing reassessment keeps care safe and responsive to the senior’s evolving condition.
What Qualifications and Training Do Philadelphia In-Home Caregivers Have for Chronic Illness Support?
Philadelphia in-home caregivers who support chronic illness commonly hold certifications and trainings that confirm clinical basics and condition-specific skills. Typical credentials include home health aide training and certified nursing assistant (CNA) preparation, plus employer-provided modules on diabetes care, fall prevention, safe transfers, and medication oversight. Care quality relies on ongoing in-service training, clinical supervision, and documented competency checks that reinforce disease-specific skills. This commitment to better training leads to better care for seniors. Knowing how credentials map to practical tasks helps families assess caregiver readiness for more complex chronic-care needs.
To show how certifications connect to hands-on skills, the table below outlines common credentials and their relevance to chronic disease care.
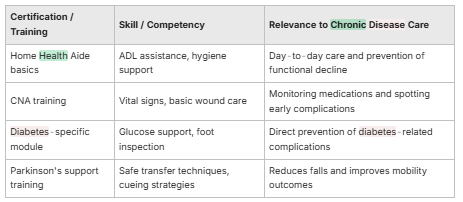
Which Certifications Ensure Quality Chronic Disease Care?
Foundational certifications like home health aide training and CNA credentials show core abilities for assisting with ADLs, checking vitals, and performing basic wound care — all important for chronic disease support. Specialized modules in diabetes management, fall prevention, and swallowing safety add targeted skills that lower condition-specific risks. Families should look for documented competency checks, supervised field experience, and continuing education records to ensure caregivers stay current with best practices. These verification steps are strong indicators that a caregiver can safely support a senior with complex needs.
How Do Caregivers Stay Updated on Chronic Disease Management Best Practices?
Caregivers stay current through continuing education, in-service trainings by clinical staff, case-review partnerships with clinicians, and routine competency refreshers that include guideline updates and new remote-monitoring technology. Agencies typically schedule periodic trainings on topics like updated diabetes protocols, fall-prevention strategies, and effective telehealth use, and they use supervision and peer mentoring to translate learning into daily practice. This ongoing learning cycle helps ensure caregivers apply evidence-informed approaches in home settings.
The Role of Caregivers in the Remote Management of Type 2 Diabetes
Remote patient management captures real-time health data and sends it to clinicians to support care decisions. The use of remote-monitoring technologies has grown in recent years, offering real-time outcome assessment and reducing clinic visits. These tools became more widespread during the COVID-19 pandemic and highlight caregivers’ important role in supporting remote monitoring for people with type 2 diabetes.
Where Can Philadelphia Families Find Local Resources and Support for Senior Chronic Disease Care?
Philadelphia families can draw on city programs, community senior centers, disease-specific support groups, and clinics with geriatric expertise to strengthen in-home care plans. Public-health initiatives offer screenings, vaccinations, and referrals; senior centers provide meals and social activities that address social needs; and local clinics and specialists offer coordinated care and telehealth that work with in-home monitoring. Matching resources to a senior’s clinical and social needs helps families build a comprehensive support network. For more information or to get started, you can contact us directly.
Integrated Telehealth and Telecare for Chronic Disease Monitoring in the Elderly
Integrated telehealth and telecare approaches can help monitor frail elderly people with chronic diseases by linking remote data with clinical care and community supports.
What Philadelphia Senior Health Programs Support Chronic Disease Management?
Philadelphia runs programs that support seniors through screenings, nutrition assistance, transportation help, and social services to combat isolation and access barriers. Caregivers can connect seniors to meal programs tailored to dietary needs, transportation for medical visits, and public-health initiatives offering preventive care. Eligibility and enrollment vary, so caregivers who document needs and benefits can speed access; coordinating with case managers or social workers also improves timely enrollment. These program connections extend the reach of in-home care and fill social and clinical gaps.
Which Support Groups and Medical Facilities Are Available for Seniors?
Philadelphia offers disease-specific support groups and medical centers focused on geriatric and chronic-disease care where caregivers can refer seniors for specialist evaluation and peer support. Support groups — in-person and virtual — provide education, caregiver strategies, and emotional support for conditions like Parkinson’s and diabetes; major clinics offer specialty care, rehab services, and care coordination. Caregivers should keep a curated list of groups and facilities that match a senior’s needs and preferences and document referral steps to simplify appointments and follow-up. These connections help ensure medical needs are met while social supports improve adherence and well-being.
Susan Benjamin — owner of Home Matters Caregiving and a local small-business operator who also sells nostalgic, historical treats in the community — shares this family-focused view to underline how neighborhood ties and simple comforts can support seniors. From her experience, pairing clinical supports with familiar gestures and community touchpoints helps seniors feel seen and cared for. Home Matters Caregiving aims to honor that balance by offering practical advice and linking families to neighborhood resources that strengthen care plans.
Susan Benjamin, Owner — Home Matters Caregiving
Frequently Asked Questions
What role do family members play in supporting in-home care for seniors with chronic diseases?
Family members are essential partners. They join care planning, offer emotional support, and help with daily tasks. Sharing knowledge about routines, preferences, and health changes helps caregivers deliver better, more personalized care. For additional guidance, consider working with your aging coach to navigate complex decisions. Families also help coordinate communication between caregivers and healthcare providers so everyone stays aligned — which improves safety and peace of mind for the senior and the household.
How can technology be integrated into in-home care for seniors?
Technology can enhance care through remote monitoring, telehealth visits, and communication tools. Wearable monitors and home devices can send vital signs to caregivers and clinicians, while telehealth reduces the need to travel for appointments. Simple communication apps let caregivers and family members share updates and coordinate schedules. Used thoughtfully, technology strengthens safety, access, and convenience for seniors with limited mobility.
What are some common challenges faced by caregivers in managing chronic diseases at home?
Caregivers commonly face emotional strain, physical demands, and system complexity. Burnout, the physical effort of assisting with mobility and ADLs, and juggling multiple medications and appointments can be overwhelming. Navigating insurance, referrals, and community resources adds another layer. Support networks, training, respite options, and clear care plans help reduce these burdens and improve care quality.
How can caregivers ensure they are providing safe and effective care for seniors?
Safe, effective care depends on following medication protocols, monitoring vital signs, and keeping open lines with clinicians. Caregivers should have appropriate training, follow documented procedures, and perform regular home safety checks. Encouraging seniors to participate in care decisions promotes autonomy and adherence, which often leads to better outcomes.
What resources are available for caregivers seeking support in Philadelphia?
Philadelphia caregivers can access local support groups, training programs, and community health services. Organizations such as the Philadelphia Corporation for Aging provide information on caregiver support, respite care, and workshops. Disease-specific groups offer education and peer support, and community centers host events focused on caregiver skills and self-care. These resources help caregivers connect, learn, and find practical assistance.
How can caregivers adapt care plans as seniors' needs change over time?
Adaptation relies on regular assessments and clear communication with family and clinicians. Schedule periodic plan reviews and update the plan after hospital discharges or noticeable changes. Document any new symptoms or functional declines and revise medications, therapy goals, or supervision levels accordingly. Being flexible and responsive keeps care relevant and effective as needs shift.


