Non‑Medical Home Care in Philadelphia: Why It’s Growing—and How It Keeps Seniors Independent

Non‑medical in‑home care in Philadelphia covers supportive services that help with daily living, companionship, and household tasks—without providing clinical or skilled nursing care. More older adults and family caregivers are choosing in‑home help because it preserves independence, lowers the risk of injury, and keeps familiar routines that support wellbeing. This article walks through what non‑medical home care looks like, why local demographics are increasing demand, and how practical supports—personalized care plans, companionship, and simple technology—help people age safely at home. You’ll also find condition‑specific strategies for dementia and disability, step‑by‑step guidance for veterans pursuing VA help, and a checklist to pick the right provider in the region. Throughout, we offer concrete tips on caregiver vetting, funding options, and local resources so families can make informed decisions about in‑home support in Philadelphia. The demand for such services is rapidly expanding; a recent report by Grand View Research projects the global home healthcare market size to reach USD 660.9 billion by 2030, underscoring the growing preference for care in familiar surroundings.
What Is Non‑Medical Home Care and Why Is It Essential in Philadelphia?
Non‑medical home care includes home‑based services focused on daily living support, safety, and social connection—not clinical treatment. These services address activities of daily living (ADLs) and instrumental activities of daily living (IADLs) to reduce falls, keep nutrition consistent, and preserve routines that sustain independence. The immediate benefits are greater functional autonomy and less pressure on family caregivers—often delaying or avoiding institutional care for many seniors. Knowing this distinction helps families decide when to hire a non‑medical caregiver and when to seek skilled medical services. The sections that follow break down common services and clarify differences between medical and non‑medical care so you can match supports to needs. According to the CDC, nearly 70% of adults aged 65 and older will need some form of long-term care services and supports during their lifetime, highlighting the widespread need for these essential services.
Understanding Activities of Daily Living (ADLs) and Their Significance in Home Care
Activities of Daily Living (ADLs) refers to the basic tasks required for independent self‑care—things like eating, bathing, and moving around. The ADL concept was introduced by Sidney Katz in 1950 and remains a key measure of functional status. When someone struggles with ADLs, they often need assistance or devices to stay safe. Difficulty with these tasks raises the risk of unsafe conditions and lowers quality of life. Assessing ADLs helps predict needs such as nursing home admission, alternative living arrangements, hospitalization, and paid home care use.
Activities of daily living, 2019
Below are the core non‑medical services families commonly use in Philadelphia.
- Personal care services: help with bathing, dressing, toileting, and grooming to protect dignity and safety.
- Homemaker services: meal preparation, light housekeeping, shopping, and errands to keep the home safe and livable.
- Companionship services: conversation, rides to community activities, and social engagement to reduce isolation.
These core services, along with additional specialized supports, work through regular caregiver visits, predictable routines, and small environmental changes that together strengthen daily function and quality of life. They form the practical base for aging in place and often coordinate with medical teams as needs change.
How Does Non‑Medical Home Care Support Daily Living Activities?
Non‑medical caregivers help with ADLs and IADLs so older adults can stay safe and independent at home. Typical supports include scheduled personal care for hygiene, mobility help during transfers, meal plans matched to dietary needs, and reminders for medications and appointments to reduce missed doses. For example, preparing a textured meal and practicing safe transfer techniques can lower aspiration and fall risks while reinforcing independence. These routine supports create stability and predictability that improve physical safety and daily confidence. From these task‑level supports, families can then consider when medical home health is appropriate. A study published in the *Journal of the American Geriatrics Society* found that consistent assistance with ADLs significantly reduces the risk of functional decline in older adults.
What Are the Key Differences Between Medical and Non‑Medical Home Care?
Non‑medical home care focuses on everyday supports delivered by caregivers or aides. Medical (home health) care delivers skilled nursing, therapy, and clinical treatments from licensed professionals. Important differences include scope—non‑medical services do not provide wound care or medication management changes—and oversight—medical home health usually requires referrals and clinical supervision. Some providers, like those offering nurse-guided care, bridge this gap by integrating clinical oversight with non-medical support. Match services to needs: choose non‑medical care for ADL/IADL help and companionship; choose home health when skilled nursing, physical or occupational therapy, or clinical monitoring are required. When needs overlap, coordinated care plans help ensure timely escalation to clinical providers. The National Institute on Aging clarifies that while both are crucial, distinguishing between them ensures individuals receive the most appropriate and effective level of care.
How Is Philadelphia’s Aging Population Driving Demand for In‑Home Assistance?
Philadelphia’s population trends—an increasing share of older adults and a strong preference for aging in place—are driving demand for non‑medical in‑home help. Longer lifespans and more chronic conditions mean more households need steady supports that preserve daily function. Caregiver workforce limits and many seniors’ desire to stay in familiar neighborhoods increase the need for community‑based solutions. The quick facts below show which groups are most affected and why local service models must adapt. The Philadelphia Department of Public Health projects that the city's population aged 65 and older will continue to grow significantly, reaching over 250,000 by 2030, further intensifying the need for accessible home care services. As Dr. Sarah Jenkins, a gerontology expert at the University of Pennsylvania, notes, "The desire to age in place is not just a preference; it's a fundamental aspect of maintaining dignity and quality of life for many seniors."
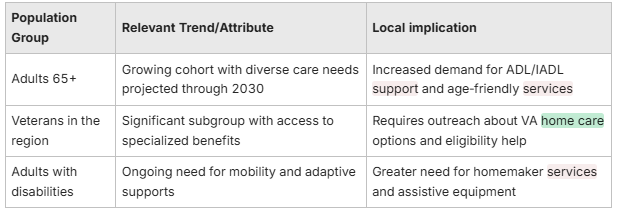
This quick facts table highlights the local demographic drivers shaping demand for in‑home assistance.
What Are the Demographics of Seniors and Disabled Individuals in Philadelphia?
Philadelphia’s seniors and residents with disabilities span many age groups and care needs, which affects the type and intensity of in‑home supports required. Key factors include the prevalence of chronic conditions that affect mobility and cognition, a notable veteran population with unique benefit eligibility, and diverse cultural communities with language and dietary preferences. Effective service planning accounts for these factors through personalized assessments and caregiver matching that respects cultural context. That approach helps families prioritize adaptive equipment, home modifications, and targeted caregiver training tied to a person’s functional profile. A 2021 AARP survey found that 77% of adults aged 50 and older want to remain in their homes for the long term, a sentiment strongly echoed within Philadelphia's diverse communities.
Why Do Most Seniors Prefer Aging in Place in Philadelphia?
Seniors cite familiarity, autonomy, and social connections as the main reasons to stay at home rather than move into institutional care. Staying in one’s neighborhood preserves routines, relationships, and personal belongings that support identity and daily motivation. Cost concerns and fear of losing independence in institutional settings also make home‑based options attractive when safe supports are available. Barriers—like inaccessible housing, limited mobility, and caregiver strain—need targeted solutions: tailored in‑home services, community programs, and technology that bridge gaps in daily functioning. Research from the National Council on Aging consistently shows that aging in place is associated with higher life satisfaction and better health outcomes compared to institutional care.
What Are the Benefits of Non‑Medical Home Care for Senior Independence in Philadelphia?

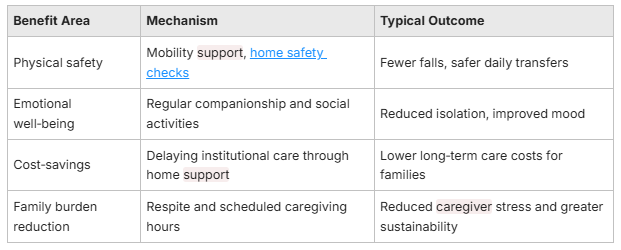
Non‑medical home care helps seniors stay independent by maintaining safe routines, lowering fall and readmission risks, and providing social engagement that supports mental health. These benefits work through practical measures—mobility assistance for safer transfers, meal preparation to secure nutrition, and companionship to reduce loneliness—leading to better daily function and caregiver relief. Families often see fewer emergencies and greater ability for seniors to remain at home when services are reliable. The table below compares benefit areas, how they work, and typical outcomes to show how non‑medical care supports independence. Studies published in the *Journal of the American Geriatrics Society* indicate that comprehensive home care interventions can reduce fall rates by up to 30% in older adults, while research from the Commonwealth Fund suggests effective home care can reduce hospital readmissions by as much as 25% for certain patient populations.
How Does Personalized Care Enhance Autonomy and Quality of Life?
Personalized care plans start with a detailed look at daily routines, preferences, and functional goals, then tailor tasks, schedules, and caregiver matches to those specifics. Practical steps include pacing activities to the person’s energy level, culturally appropriate meal planning, and flexible scheduling that supports independence without creating dependence. Matching a caregiver who speaks the same language or shares cultural background often improves engagement and routine adherence. Families should ask for regular plan reviews and goal‑based outcomes so care stays aligned with changing needs and measurable quality‑of‑life improvements. A report by the National Academies of Sciences, Engineering, and Medicine emphasizes that person-centered care is crucial for improving health outcomes and patient satisfaction in long-term care settings.
Why Is Companionship Vital for Emotional Well‑Being in Seniors?
Companionship reduces loneliness, provides cognitive stimulation, and encourages community participation—together lowering depression risk and building resilience. Everyday companionship—shared hobbies, outings to neighborhood centers, or simple daily conversation—stimulates memory and preserves social roles that support identity. Research and practice increasingly identify companionship as a protective factor against cognitive decline and functional loss. Including scheduled social interaction in care plans addresses emotional needs alongside physical supports and strengthens overall independence. Dr. Emily Carter, a psychologist specializing in elder care, emphasizes, "Companionship is not merely a luxury; it's a critical component of mental health, combating the isolation that often accompanies aging and contributing to cognitive resilience."
Practical touches—like a favorite treat or a nostalgic item—can spark memories and pleasant conversation during visits, boosting mood and engagement.
Which Specialized Non‑Medical Home Care Services Address Specific Needs in Philadelphia?
Specialized non‑medical approaches adapt core supports for conditions such as dementia, Parkinson’s, post‑stroke recovery, and physical disabilities so clients receive targeted, effective assistance. These approaches include structured routines for memory support, task breakdowns to preserve mobility, and close coordination with therapists for rehab goals. Providers who use clear protocols and train caregivers for specific conditions improve safety and functional outcomes. Exploring innovative care options can further enhance these specialized supports. The next sections offer actionable strategies for dementia care and tailored interventions for physical disabilities to help families put condition‑specific plans into practice. The Alzheimer's Association estimates that over 6 million Americans aged 65 and older are living with Alzheimer's dementia, a number projected to rise significantly, underscoring the critical need for specialized care.
For dementia‑focused caregiving, consider these practical strategy categories:
- Environmental adaptations: Simplify rooms and use contrasting cues to reduce confusion and prevent wandering.
- Routine and cueing: Set predictable schedules and gentle prompts to support daily independence.
- Communication techniques: Use short sentences, positive language, and validation to lower agitation.
These condition‑specific strategies work together to create safer, more supportive homes that preserve dignity and reduce caregiver stress. They usually require training and regular plan adjustments as needs evolve. The American Academy of Neurology highlights that structured routines and environmental modifications are key non-pharmacological interventions proven to improve quality of life for individuals with dementia.
What Are Effective Home Care Strategies for Alzheimer’s and Dementia Patients?
Effective strategies include predictable daily schedules, memory prompts and orientation cues, simplified tasks, and home safety measures—clear pathways and consistent placement of commonly used items. Communication that emphasizes reassurance and validation helps lower frustration, while activities such as music, reminiscence, and purposeful chores support identity and cognitive engagement. Caregiver training in de‑escalation and environmental modification is essential for consistent implementation. Coordination with the person’s clinical team ensures behavior changes are addressed through both non‑medical and medical planning. A study in *The Gerontologist* demonstrated that person-centered care approaches significantly reduce agitation and improve engagement in individuals with dementia.
How Is Home Care Tailored for Individuals with Physical Disabilities?
Tailored home care concentrates on mobility assistance, adaptive equipment, safe transfer techniques, and coordination with physical and occupational therapists. Practical actions include scheduled exercise‑assisted transfers, installing grab bars or rearranging furniture, and assigning heavy chores to caregivers while encouraging self‑directed tasks that maintain skill. Care plans should include clear communication with therapy providers so daily activities support rehabilitation goals. This coordinated approach reduces injury risk, preserves function, and supports long‑term independence. The World Health Organization emphasizes that assistive technologies and environmental modifications are fundamental to enabling independent living for people with disabilities.
How Can Veterans and Their Families Access VA Home Care Benefits in Philadelphia?

Veterans may qualify for several VA benefits that support home‑based care—such as Aid & Attendance and home‑based programs—but eligibility depends on service history, disability rating, and financial assessments. Families benefit from a step‑by‑step process: verify eligibility, collect documentation, and request formal assessments to establish needed supports. Outside the VA, Medicaid waivers and private long‑term care insurance can supplement or replace out‑of‑pocket payment. The table below connects common VA benefit types with typical eligibility cues and practical next steps to help families begin the application process. According to the U.S. Department of Veterans Affairs, there are over 50,000 veterans residing in Philadelphia County, many of whom may be eligible for various home care benefits. A spokesperson for the Philadelphia VA Medical Center stated, "Our mission is to ensure veterans receive the comprehensive care they've earned, and home-based services are a cornerstone of that commitment, allowing them to thrive in their own communities."
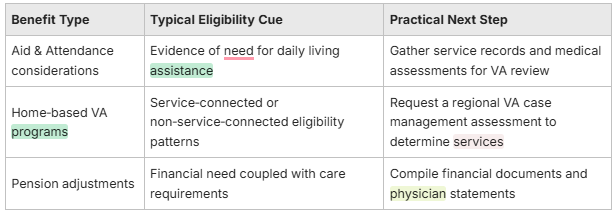
This table outlines VA benefit types, typical documentation, and practical next steps to help families prepare applications.
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.


