Signs Your Loved One Needs Non-Medical In-Home Care in Philadelphia: How to Recognize When to Get Help

Recognizing when a senior needs non-medical in-home care in Philadelphia starts with observing daily patterns that affect safety, nutrition, medication, and social connection. According to the AARP, nearly 90% of adults over age 65 want to stay in their homes as long as possible, underscoring the importance of timely and appropriate in-home support. The U.S. Census Bureau projects that by 2030, all baby boomers will be older than 65, significantly increasing the demand for senior care services, particularly in-home options. This article explains what non-medical in-home care means, why early detection preserves independence (learn more about why home matters), and how simple observations translate into practical next steps for families and caregivers. You will learn the most common signs to watch for, how to use a home care assessment checklist, how to spot fall and mobility risks at home, and when to seek respite or community resources in the Philadelphia area. The guidance below emphasizes concrete checks you can perform at home, red flags that warrant a professional assessment, and local support pathways, including caregiver respite and funding options. Throughout, we use keywords relevant to senior assistance Philadelphia and non-medical home care Philadelphia to make this a practical, local-first guide you can act on immediately. For comprehensive local support, visit Home Matters and explore our full range of caregiver services.
What Are the Most Common Signs Your Elderly Loved One Needs In Home Care?
Non-medical in home care refers to assistance with daily living tasks and companion support rather than clinical medical treatment, and it helps maintain safety, nutrition, and routine in a familiar environment. Studies show that approximately 30% of adults aged 65 and older require assistance with at least one activity of daily living (ADL), highlighting the widespread need for such support. For a full list of available assistance, explore our caregiver services. Early recognition focuses on declines in activities of daily living and instrumental tasks, worsening medication adherence, increasing fall incidents, and changes in hygiene or weight. Spotting these patterns early reduces emergency risks and preserves independence, allowing families to arrange tailored companion care or personal care in time. The National Council on Aging reports that medication non-adherence costs the U.S. healthcare system an estimated $300 billion annually due to avoidable hospitalizations and complications, while the CDC states that one in four Americans aged 65 and older falls each year, making falls the leading cause of injury and death in this age group. The list below highlights the most actionable, observable signs families commonly miss and serves as a quick diagnostic checklist to decide whether to pursue a formal home assessment next.
Common signs that suggest an immediate conversation about care is needed:
- Decline in basic ADLs: Regular difficulty with bathing, dressing, or toileting that was not present before.
- Trouble with IADLs: Missed bill payments, neglected grocery shopping, or inability to manage transportation.
- Medication mismanagement: Missed doses, duplicate doses, or confusion about what to take and when.
- Repeated falls or near-falls: Any fall or frequent stumbling increases near-term injury risk.
- Changes in hygiene or weight: Unwashed clothing, poor grooming, or noticeable weight loss over weeks.
- Withdrawal and missed appointments: Social isolation, skipped medical visits, or missed social engagements.
- New or worsening confusion: Reorientation problems, repeated questions, or trouble following familiar routines.
- Home environment degradation: Untidy living spaces, expired food, or safety hazards that accumulate.
These signs form a practical snapshot you can use at home to decide whether to arrange extra help or schedule a professional home safety assessment next. Observing one warning sign may merit monitoring, while multiple concurrent signs typically indicate the need for timely in-home support.
Intro to a comparison table: To help prioritize actions, the table below summarizes common signs, how often they occur, and immediate recommended actions families can take before or while arranging formal care.
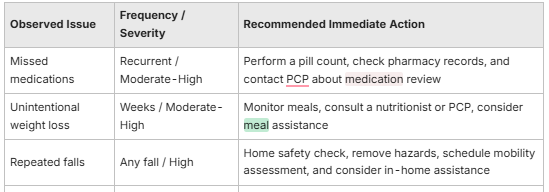
This comparison helps families assess urgency and choose immediate steps such as medication checks, arranging meal support, or scheduling a home safety review. Use these actions as a bridge to a fuller home care assessment when multiple items appear together.
How Does Decline in Activities of Daily Living Indicate Need for Care?
Activities of daily living (ADLs) are the core personal tasks — bathing, dressing, toileting, transferring, continence, and feeding — while instrumental activities of daily living (IADLs) include managing finances, preparing meals, shopping, and transportation. A decline occurs when a once-independent person needs prompting, repeated help, or cannot complete tasks safely, and this loss of function directly increases risk of malnutrition, falls, and social isolation. For example, unwashed clothing, missed meals, and unpaid bills are concrete indicators that IADLs are slipping; when those accumulate, arranging in-home companion or personal care reduces immediate risk. Research published in the Journal of the American Geriatrics Society indicates that a decline in IADLs often precedes ADL decline and is a strong predictor of future care needs. A 2017 study in the journal *Health Affairs* further found that older adults who receive in-home care are 25% less likely to be hospitalized for preventable conditions. A brief family checklist can help decide when to act: note frequency of missed tasks, whether assistance prevents harm, and whether the pattern is new or progressive.
Families can use a simple scoring approach: one missed ADL per week suggests monitoring, two or more recurring missed ADLs suggests arranging in-home support. This scoring leads naturally to checking medication management and safety hazards, which are common concurrent problems.
Research indicates that home-based assessments are a preventative strategy to identify and meet service needs, particularly non-medical ones, within the elderly population.
Home Assessments Identify Non-Medical Needs in Older Adults
Our findings support and expand upon previous reports regarding the utility of unsolicited home assessments in identifying unmet needs, particularly non-medical ones, within the elderly population.
Home‐based assessment for family carers: a preventative strategy to identify and meet service needs, H Herrman, 1997
What Are Red Flags in Medication Management and Adherence?
Medication mismanagement is a high-risk area because it can cause acute events or accelerate decline; red flags include missed doses, pill duplication, expired medications in use, or visible confusion about regimens. It's estimated that medication non-adherence contributes to approximately 125,000 deaths and 10% of hospitalizations annually in the U.S. (Source: Centers for Disease Control and Prevention). Practical family checks include counting pills weekly, reviewing medication lists with the prescribing pharmacy, and observing for side-effect behaviors such as drowsiness, agitation, or frequent falls after new prescriptions. If you find missed or duplicated doses, call the prescriber to clarify the regimen and consider short-term in-home support for medication reminders, or explore options for nurse-guided care. For comprehensive assistance, explore our medication assistance services. Regular caregiver visits or medication reminder services reduce these risks and provide an opportunity for a professional to report concerning trends to clinicians. A study in the American Journal of Managed Care found that up to 50% of older adults do not take their medications as prescribed, underscoring the prevalence of this issue.
Addressing medication issues often reveals mobility or cognitive problems that warrant a safety assessment and possibly ongoing non-medical caregiving, creating a clear rationale for arranging a structured home care evaluation.
Studies have explored the variability in measuring functional decline in activities of daily living, with observed decreases in functional level reported in various contexts.
Quantifying Functional Decline in Activities of Daily Living Among Older Adults
Variability in the measurement of (instrumental) activities of daily living functioning and functional decline in hospitalized older medical patients: a systematic review. In studies employing the Katz ADL index, the minimal observed decline ranged from a 3.6% to 20% decrease in functional level [9], [10], [12].
Variability in measuring (instrumental) activities of daily living functioning and functional decline in hospitalized older medical patients: a systematic review, BM Buurman, 2011
When Is the Right Time to Get Non-Medical Home Care for Seniors in Philadelphia?
Determining the right time for non-medical home care balances sustained decline, immediate safety risks, and the caregiver’s capacity to provide consistent support without compromising health. A significant majority, 87%, of adults age 65 and older want to stay in their current home and community as they age, underscoring the importance of timely in-home support. The National Association for Home Care & Hospice (NAHC) highlights that home care can reduce hospital readmissions by 25% and delay nursing home placement by an average of 1.5 to 2 years. In practical terms, persistent difficulty with two or more ADLs or IADLs, repeated falls, worsening medication adherence, or caregiver burnout are strong criteria indicating it’s time to arrange professional 1-on-1 personalized in-home assistance. Scheduling a professional home assessment provides an objective evaluation and care plan tailored to the Philadelphia household environment, helping families prioritize safety fixes, companionship, or personal care hours. To learn more about our approach to personalized care, visit our About Us page. The decision flow below is designed to help families move from observation to action, including when to seek respite and how to prepare for a formal assessment.
How to use a checklist: Use scoring thresholds where increasing counts of missed tasks or safety incidents move you from monitoring to arranging scheduled caregiver visits. This checklist approach ensures decisions match observed needs and caregiver capacity, and can be tailored with care on your schedule.
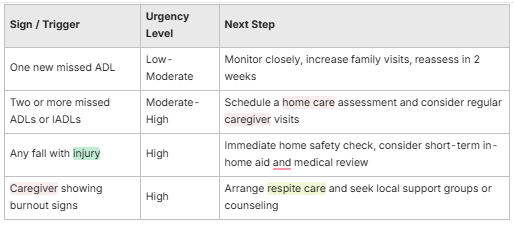
This decision table helps families prioritize immediate actions and plan for transitional support such as companion care, respite, or structured personal care hours. Once urgency is established, the next step is a targeted home care assessment to detail specific tasks and a schedule.
How to Use a Home Care Assessment Checklist to Decide?
A home care assessment checklist converts observations into quantifiable needs by scoring ADLs, IADLs, medication management, nutrition, and home safety hazards. Comprehensive geriatric assessments have been shown to improve functional status and reduce mortality in older adults, highlighting the value of structured evaluations (Source: Cochrane Database of Systematic Reviews). The American Geriatrics Society recommends regular comprehensive assessments for older adults to proactively identify and address health and social needs. To use it, walk through the home with the checklist, record frequency of missed tasks, note environmental risks, and rate caregiver capacity on a simple scale; this score guides whether to pursue part-time visits, daily companionship, or more intensive personal care. Many families find that interpreting a composite score clarifies next steps: low scores suggest monitoring with increased family involvement, moderate scores suggest scheduled caregiver visits, and high scores indicate immediate professional in-home support. The assessment also produces a prioritized action list for repairs, mobility aids, and scheduling support that you can share with clinicians or care agencies.
After completing the checklist, the logical next step is a local resource review to find providers who can meet the documented needs and to explore funding options for ongoing support. Visit our resources page for more information, or learn about our innovative care options.
What Are Early Warning Signs That Should Prompt Action?
Early warning signs that often precede larger declines include unexplained weight loss, missed medical appointments, new episodes of confusion, and social withdrawal from friends and activities. These subtle indicators frequently show up before falls or severe medication errors, and acting on them promptly can prevent escalation into emergency situations. Early intervention with non-medical home care can delay or prevent the need for more intensive care settings by an average of 1.5 to 2 years (Source: National Association for Home Care & Hospice). Immediate recommended actions include increasing visit frequency, documenting occurrences with dates and examples, and scheduling a professional home safety review or primary care evaluation. Addressing early signs quickly preserves options for less-intensive interventions like companion care rather than later requiring more extensive supports.
Documenting these early warning signs and communicating them to the clinician or assessor sets the stage for an effective, preventative care plan.
How Can You Identify Safety Risks and Mobility Issues at Home?
Identifying safety risks and mobility decline focuses on observable movement changes and environmental hazards that increase fall risk, along with straightforward mitigation steps families can take immediately. Falls are the leading cause of injury and death among older Americans, with over 3 million older adults treated in emergency departments for fall injuries annually (Source: CDC). Common household hazards include loose rugs, poor lighting, cluttered walkways, and a lack of grab bars in bathrooms; recognizing these encourages low-cost modifications that dramatically reduce fall likelihood. According to the National Institute on Aging, simple home modifications, such as installing grab bars and improving lighting, can reduce fall risk by up to 30%. Functional mobility signs — slower gait, using furniture to rise, or needing one hand for balance — indicate reduced stability and a need for mobility-focused supports. A short home safety walkthrough and mobility observation test provide actionable evidence to decide whether to schedule assistive devices, physical therapy, or regular in-home assistance. For specific strategies, explore our fall prevention resources. The financial cost of falls for older adults is substantial, with medical costs totaling over $50 billion annually (Source: CDC).
After identifying hazards and mobility limitations, prioritize fixes that address immediate risks and plan for professional assessments if mobility tests show decline.
A review of fall risk assessment tools highlights the importance of evaluating multifactorial and functional mobility assessment tools for older adults in various care settings.
Fall Risk Assessment Tools for Older Adults in Home Care Settings
This review discusses the most appropriate fall-risk assessment tool(s) for the risk profile of older adults across community, home-support, long-term, and acute care settings. The objective is to identify and evaluate the validity and reliability of multifactorial and functional mobility assessment tools for fall risk among individuals aged 65 years and older.
Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings, J Close, 2007
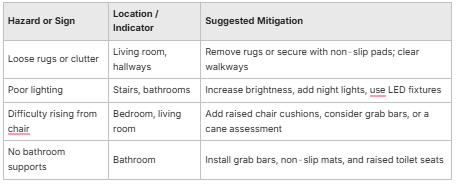
This hazard-to-mitigation mapping helps families prioritize inexpensive, high-impact changes and determine when to bring in professionals for stair lifts or broader remodeling. Early fixes often prevent falls and delay the need for more intensive care.
What Are the Key Indicators of Fall Hazards and Mobility Decline?
Key indicators of mobility decline include slowed walking speed, reduced endurance, frequent reliance on furniture for support, and a history of near-falls; these functional signs often precede an actual fall. Simple tests families can observe are whether the person rises from a chair without using hands, how long a short walk takes, and whether balance recovers after a small perturbation; failing these suggests a mobility evaluation is warranted. Environmental indicators such as stairs without handrails, cramped bathrooms, and multi-level living spaces further increase fall risk regardless of baseline function. Noting these indicators together creates a clear case for scheduling mobility aids, home modifications, or regular caregiver support focused on safe transfers.
Observing mobility decline and environmental hazards together usually triggers a home safety assessment and discussion of supports like supervision during transfers or scheduled caregiver visits.
How to Conduct a Home Safety Assessment Checklist in Philadelphia?

A room-by-room home safety checklist tailored to urban Philadelphia housing highlights stairs, carpeting transitions, bathroom setups, and entryway clutter as common local concerns; start by documenting problem areas and photographing them for a repair plan. Walk each room with a simple checklist that covers lighting, trip hazards, bathroom supports, stair handrails, and furniture stability, and rate each item as safe, caution, or unsafe to prioritize fixes. Record findings in a single document to share with contractors, clinicians, or a home assessor and schedule high-priority fixes such as grab bar installation or brighter lighting first. Local aging services and community volunteer programs often assist with minor modifications, so documenting needs clearly increases the likelihood of timely help. For additional guidance and tools, check our resources.
Completing the checklist naturally leads to calculating a prioritized budget and exploring local funding or volunteer options to implement the most urgent safety changes.
How Does Social Isolation and Mood Changes Signal the Need for Home Care?
Social isolation and mood changes are powerful predictors of functional decline and increased health risks; when seniors withdraw, experience persistent low mood, or lose interest in daily activities, their physical health and safety often deteriorate. Research indicates that social isolation in older adults is associated with a 50% increased risk of dementia and a 29% increased risk of heart disease (Source: National Academies of Sciences, Engineering, and Medicine). The World Health Organization recognizes social isolation as a significant public health concern, comparable to obesity and smoking in its impact on health outcomes. Non-medical home care can provide companionship, structured social activities, and help maintain routines that counteract loneliness and depressive symptoms. Discover how our Aging Coach can provide guidance and support. Observing decreased communication, missed social events, or changes in sleep and appetite signals the need for engagement-focused support rather than strictly physical assistance. Addressing social factors early improves adherence to medications and appointments and often delays the need for more intensive care by restoring meaningful daily structure. A study by the University of Chicago found that loneliness can increase the risk of premature death by 14%, emphasizing the severe impact of social isolation.
Small, consistent social interventions frequently have outsized effects on mood and engagement and serve as an entry point to broader in-home support planning.
Families can use small, meaningful gestures to improve mood and social engagement, such as bringing favorite snacks or nostalgic treats during visits, inviting participation in familiar hobbies, or coordinating regular check-ins to rebuild routine. These low-cost actions increase visits' emotional value and can make formal companion care more effective by reinforcing familiar sensory cues and memories. Susan Benjamin, owner of True Treats Candy, notes that bringing a nostalgic treat during transitions can spark conversation and comfort for a senior adjusting to in-home support. Integrating small comforts during visits helps bridge to longer-term companionship arrangements and improves responsiveness to broader care plans.
What Are Signs of Loneliness and Depression in Seniors?
Signs of loneliness and depression in older adults include social withdrawal, loss of interest in hobbies, sleep and appetite changes, and expressions of hopelessness or persistent sadness; physical complaints without clear medical cause can also signal mood issues. The National Institute of Mental Health estimates that over 2 million Americans aged 65 and older suffer from depression, a condition often exacerbated by loneliness. Family members should track changes in activity level, missed social contacts, and alterations in personal care as potential indicators of low mood. Immediate family actions include increasing supervised visits, encouraging participation in community activities or senior centers, and consulting the primary care provider for assessment when mood changes persist. Early social engagement and structured companionship often reverse mild depressive patterns and reduce downstream risks such as poor nutrition or medication nonadherence.
Recognizing mood changes early allows families to pair companionship visits with other supports such as meal assistance or transportation to social events, improving overall outcomes.
How Can Non-Medical Care Help Improve Social Engagement?

Non-medical caregivers provide conversation, shared activities, and community outings that restore routine and meaningful interaction, with outcomes including improved mood, better nutrition, and increased adherence to daily tasks. Learn more about our social engagement services. Typical companion activities include conversation and memory prompts, escorting to appointments, facilitating hobbies, and supervised walks or outings that encourage mobility and social contact. Regular, scheduled visits create predictable social rhythm that reduces anxiety and loneliness and offers caregivers opportunities to observe emerging safety concerns and report them to family members. Our care team is dedicated to providing compassionate and consistent support. In many cases, a combination of volunteer programs and paid companion visits creates a hybrid approach that sustains social engagement while managing costs.
Improved social engagement from companion care often reduces the immediate need for higher-cost personal care and provides a bridge to other community services that support long-term well-being.
What Support Options Are Available for Family Caregivers in Philadelphia?
Family caregivers in Philadelphia have access to a mix of respite models, community programs, and national resources that help balance caregiving duties with personal health; knowing where to look and how to qualify matters for timely access. In Pennsylvania, there are approximately 1.6 million family caregivers providing an estimated 1.4 billion hours of care annually, valued at $19.6 billion (Source: AARP, Valuing the Invaluable 2023 Update). Respite care ranges from short hourly in-home visits that provide family breaks to scheduled day programs that combine social engagement and supervision; families should evaluate options based on frequency needed and the senior’s comfort with new people in the home. Local aging services and national organizations like AARP can provide referrals, printed checklists, and guidance on available programs and eligibility, while community nonprofits sometimes offer targeted assistance for low-income households. Recognizing caregiver burnout early and using these support options preserves family health and prevents crisis-driven care transitions. Learn more about our commitment to better training and better care.
Below is a practical list caregivers can use to identify immediate supports and where to start when searching for local assistance.
- Hourly respite services: Short-term caregiver visits to give family members scheduled breaks.
- Adult day programs: Structured daytime social and therapeutic activities for seniors.
- Support groups and counseling: Peer groups and mental health support for caregiver stress.
- Volunteer assistance programs: Community volunteers who help with errands or home modifications.
Using the list above, caregivers can prioritize immediate relief (hourly respite) and longer-term solutions (day programs), documenting preferences and schedules to share with providers. Scheduling a mix of supports reduces burnout risk and makes ongoing in-home care more sustainable.
Susan Benjamin, owner of True Treats Candy, offers a practical note for families: small gestures like bringing historically familiar treats can be a comforting addition when caregivers visit or when scheduling respite, providing emotional continuity during transitions. This suggestion is intended as a low-cost, high-impact way to support social engagement and does not represent medical advice or caregiving services.
How to Recognize Caregiver Burnout and When to Seek Help?
Caregiver burnout shows as chronic fatigue, sleep disturbance, irritability, feelings of resentment, and declining physical health; it often appears gradually and can undermine the ability to provide safe care. Studies show that up to 40% of family caregivers experience symptoms of depression, highlighting the critical need for respite and support (Source: Family Caregiver Alliance). The National Alliance for Caregiving reports that caregivers who experience burnout are more likely to suffer from chronic health conditions themselves. A short self-checklist helps caregivers gauge risk: persistent exhaustion despite rest, neglecting personal health, increased frustration toward the care recipient, and withdrawing from social supports are clear red flags. Immediate steps include arranging short-term respite, contacting local support groups, delegating specific tasks, and seeking counseling or primary care evaluation for stress-related symptoms. Prioritizing caregiver health safeguards the senior’s well-being and allows families to transition to sustainable care models before emergencies occur.
Taking these steps leads naturally to exploring local funding and referral options to offset costs and secure ongoing support.
What Local Resources and Funding Options Support In Home Care?
Philadelphia families can explore a mix of state and city programs, nonprofit grants, and national resources that help offset in-home care costs or to find referrals; start by contacting local aging service organizations and national associations for eligibility guidance, or check our online resources and information on paying for home care. Common pathways include community-based grants for home modifications, subsidized transportation services for medical appointments, and referral directories that list vetted respite and companion services. National entities such as AARP provide printed guides and advocacy information, while local agencies may offer targeted programs for low-income seniors or veterans’ services for eligible households. When researching options, document eligibility criteria and required paperwork to streamline applications and match funding to priority needs like home safety fixes or short-term respite. For specific guidance on conditions like Parkinson's, refer to our home care assistance tips for Parkinson's.
Organizing resource contacts and eligibility notes in a single folder or digital file makes it easier to apply for support when needs escalate and ensures timely access to possible funding sources.
How Much Does Non-Medical Senior Home Care Cost in Philadelphia?
Non-medical home care pricing in Philadelphia varies with hours per week, level of assistance, travel time, and whether care is scheduled hourly or as a live-in arrangement; these factors determine whether families pay for a few hours of companion care or daily personal assistance. According to the Genworth Cost of Care Survey 2023, the median cost for non-medical home care (homemaker services) in the Philadelphia area is approximately $28 per hour, with personal care services slightly higher. Typical cost drivers include the number of ADLs requiring help, frequency of visits, specialized tasks like mobility transfers, and agency overhead such as background checks and training. Estimating monthly costs starts with calculating the needed hours per week and multiplying by local hourly rates, while adding transportation or mileage fees where applicable. For those in surrounding areas, we also offer live-in care in West Chester, PA, Phoenixville, PA, and Chester, PA. The table below summarizes common cost-influencing factors and sample ranges to help families form a realistic budget and ask informed questions of providers.
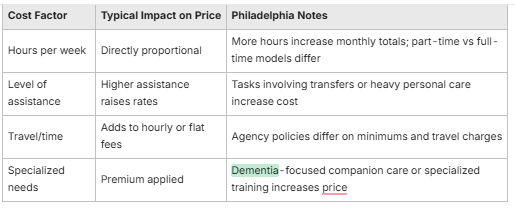
This comparison clarifies why two similar-looking care plans can differ in price and underscores the importance of getting itemized estimates from providers. Asking for clear hourly versus package pricing and any minimum shift lengths helps families control costs.
What Factors Influence Home Care Pricing in Philadelphia?
Primary factors that influence pricing include whether care is hourly or live-in, the complexity of tasks required (e.g., assistance with transfers vs. companionship), caregiver qualifications, and agency administrative fees. Hourly care offers flexibility for short-term needs or respite, while live-in care involves different billing structures that often include room and board considerations and different regulatory factors. Ask providers about minimum shift lengths, cancellation policies, overtime rates, and whether training or specialty care (memory care, mobility assistance) is reflected in the hourly rate. Clear questions about these factors yield apples-to-apples comparisons and help families choose a model that balances support and affordability.
Understanding pricing drivers prepares families for productive conversations with agencies and aligns care selections with the documented needs from your home care assessment.
Are There Financial Assistance Programs for In-Home Care?
Financial assistance options may include community grants for home modification, subsidized transportation, veterans’ benefits where eligible, and referral services that connect families to sliding-scale programs; eligibility varies by program and household income. National organizations and local aging services offer guidance on where to apply and what documentation to prepare, while some nonprofits prioritize aid for urgent safety fixes that help seniors remain at home. Families should compile basic financial and medical documentation to speed applications and consult local aging service navigators who can point to current programs. When assistance is unavailable, creative cost strategies include combining volunteer supports, short-term respite with family coverage, and negotiating flexible schedules with agencies to reduce expense.
Exploring assistance early often reveals options that prevent costly hospitalizations or premature nursing home placement by addressing safety and respite needs when they first arise.
Susan Benjamin Owner, True Treats Candy — Susan Benjamin writes from a community-minded perspective and notes that small, nostalgic treats can provide comfort during care transitions; True Treats Candy offers unique historical and nostalgic candy selections intended to uplift families and visiting caregivers in Philadelphia.
Ready to Discuss Your Loved One's Care Needs?
Understanding pricing drivers prepares families for productive conversations with agencies and aligns care selections with the documented needs from your home care assessment. For any further questions, please visit our FAQs or contact us directly to discuss your specific needs and explore our additional services.


