Post-Hospital Care in Philadelphia: Helping Families Make a Safe, Smooth Transition from Hospital to Home

A safe hospital-to-home transition lowers complications, supports recovery, and reduces the chance of avoidable readmission for Philadelphia families managing post-acute needs. This guide breaks down what post-hospital support looks like in our city, why neighborhood factors matter, and how coordinated transitional care — from medication reconciliation to timely follow-up and home-based therapy — improves outcomes. You’ll find a practical discharge-planning checklist, a clear comparison of home equipment and setup, plain-language descriptions of in-home skilled nursing and therapy, and tips for choosing a local agency. Tables, step-by-step lists, and technology notes give caregivers concrete actions to take. We also use search-friendly terms like "hospital to home care PA" and "transitional care Philadelphia" so caregivers can find and act on this information quickly.
What Is Post-Hospitalization Support and Why Is It Essential in Philadelphia?
Post-hospitalization support is coordinated care after discharge that helps someone recover safely at home by connecting hospital treatment with in-home services. Care coordination is the core: providers confirm medications, arrange follow-up visits, and set up nursing or therapy so problems are spotted and managed before they require readmission. The results are measurable — better medication adherence, quicker functional gains, and fewer ER visits — which matters especially in Philadelphia, where transit, building layouts, and caregiver availability can affect recovery. Knowing these basics helps families prioritize discharge tasks and choose services that fit both medical needs and household realities.
Local, neighborhood-aware support is most effective: it accounts for transit time to clinics, nearby outpatient services, and community resources that complement home care. The list below highlights the main benefits so the value of transitional care is clear before we review how it works in practice.
Post-hospitalization support delivers three primary benefits:
- Readmission prevention: Medication reconciliation and early follow-up reduce avoidable returns to the hospital.
- Faster functional recovery: Home-based therapy and skilled nursing speed mobility gains and wound healing.
- Caregiver readiness: Education and respite options strengthen family members’ ability to manage day-to-day needs.
These outcomes explain why coordinated transitional care should be part of discharge planning and how those processes help prevent readmissions.
How Does Transitional Care Prevent Hospital Readmissions?

Transitional care prevents readmissions by spotting and fixing post-discharge risks — medication mistakes, missed follow-ups, or worsening symptoms — through structured check-ins and monitoring. Medication reconciliation cuts dosing errors by comparing hospital prescriptions with home regimens. Early follow-up visits catch complications before they escalate. Care coordination names who’s responsible — a case manager, nurse, or clinician — to track progress and respond to warning signs, which significantly lowers emergency returns. For Philadelphia families, arranging a primary care or specialist visit within seven days of discharge and verifying medication instructions are practical steps that reduce early complications.
Medication Reconciliation: A Key Strategy to Improve Transitional Care
Bridging the Gap in Transitional Care: An In-depth Examination of Medication Reconciliation
Accurate meds, timely clinic access, and active monitoring work together — which raises the next question: who does each task, and how do families fit into the team?
Who Are the Key Caregivers and Medical Professionals Involved?
Safe transitions are a team effort: the patient and family caregiver, the hospital discharge planner or case manager, home health nurses, physical and occupational therapists, social workers, and the primary care doctor or specialists. Family caregivers handle daily tasks and watch for changes; skilled professionals provide clinical care such as wound management, IV therapy, and rehabilitative training. Social workers and case managers arrange community services, transportation, and benefits checks so logistics don’t block recovery. Clear role definitions and a named contact from the hospital or home-care team make communication easier and improve outcomes because responsibility is assigned before discharge.
Knowing these roles helps families ask focused questions at discharge and prepares them for the practical work of care at home.
If you’re exploring local hospital-to-home options, Home Matters Caregiving can help explain hospital-to-home coordination and available services; ask your discharge planner for referrals to community programs and in-home providers.
How to Prepare for a Successful Hospital to Home Transition in Philadelphia?
A smooth transition starts with pre-discharge planning, clear communication, and a home that supports mobility and medical needs. First, confirm discharge instructions, medications, and follow-up appointments. Second, assess the home and secure needed equipment. Third, arrange in-home services and transport for timely clinic visits. This proactive approach removes common barriers to following the care plan. In Philadelphia, also plan around neighborhood specifics like stairs, elevator schedules, and local pharmacy hours.
The checklist below organizes the must-do pre-discharge tasks and explains why each matters before the patient leaves the hospital.
Essential pre-discharge checklist for families:
- Confirm the discharge summary and written care instructions: Make sure activity limits, wound/device care, and red-flag symptoms are documented.
- Verify medications and pharmacy access: Reconcile hospital prescriptions with home meds and arrange affordable pickup or delivery.
- Schedule follow-up appointments and secure transport: Book primary care or specialist visits within 7–14 days and confirm reliable transportation.
This checklist lays out immediate next steps. The equipment choices that follow determine whether the home supports safe recovery or creates extra risk.
To make equipment decisions easier, review the table below comparing common home-prep items by type and purpose.
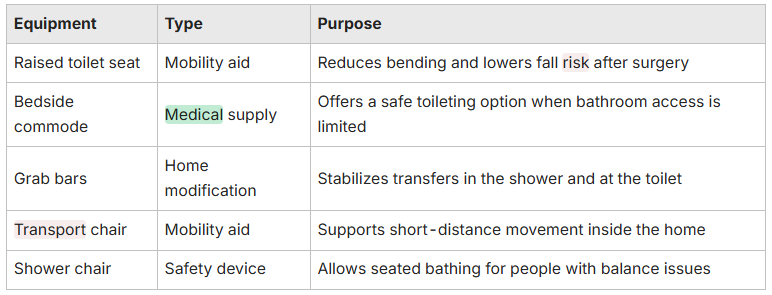
Use this table to prioritize purchases or rentals that reduce fall risk and help with daily tasks. Next, consider room-by-room setup and tips for caregivers.
What Should Families Include in a Discharge Planning Checklist?
A discharge checklist should group items into medical, logistics, and home-prep categories so families can tick off each area before leaving the hospital. Medical items include the final medication list, wound or device care instructions, emergency signs, and a schedule for follow-up visits. Logistics cover prescriptions, home health referrals, insurance authorizations, and transport. Home-prep focuses on accessibility, essential supplies, and caregiver assignments. A single organized checklist reduces mistakes and gives families a clear sequence to follow during the hectic discharge process.
Use the steps below as a straightforward sequence to prepare at discharge.
Step-by-step discharge checklist:
- Get written discharge instructions and confirm follow-up appointments.
- Reconcile all medications and arrange pharmacy pickup or delivery.
- Confirm home health or therapy referrals and verify insurance authorizations.
- Prepare the home, line up caregiver support, and gather needed supplies.
Follow these steps during discharge and in the first days at home to reduce confusion and prevent problems.
How to Prepare the Home Environment for Recovery?

Preparing the home means finding hazards, improving accessibility, and staging supplies so the recovering person can manage daily activities safely. Focus on high-risk areas — bathroom, bedroom, and stairs. Install grab bars, secure loose rugs, move furniture to create clear paths, and keep frequently used items at waist height to avoid bending. If you need a temporary ramp or mobility device, arrange rentals early and practice transfers with a caregiver before discharge. A prepared home reduces falls and conserves energy, making therapy and medication plans more effective.
Below is a short equipment comparison to guide choices and show how each item supports recovery and caregiver tasks.
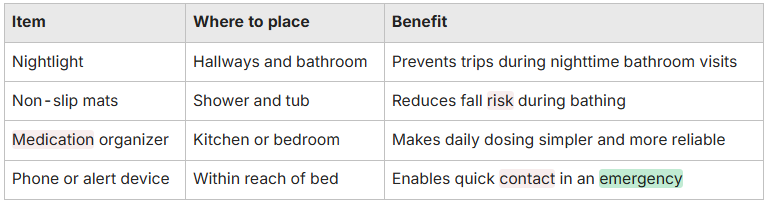
Combine these measures with caregiver training on safe transfers and medication checks to create a safer, more manageable recovery plan.
What In-Home Care Services Support Recovery After Hospital Discharge?
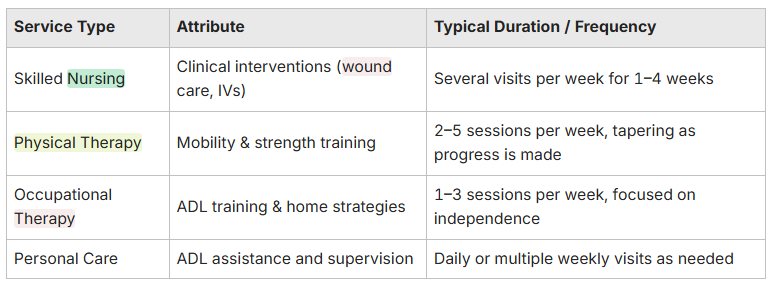
In-home care covers skilled nursing, physical and occupational therapy, medication management, and personal care — each addressing specific post-discharge needs to support clinical recovery and daily life. Skilled nurses handle wound care, IVs, and vital-sign monitoring. Therapists work on mobility, strength, and adaptive strategies to restore independence. Personal care helps with bathing, dressing, and meals while the patient regains strength. Coordinating these services with the patient’s physician ensures continuity and aligns home care with discharge goals. The right mix depends on diagnosis, current function, and recovery objectives.
The table below compares common service types with typical duration and frequency so families know what to expect early in recovery.
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.
This comparison helps families and discharge planners set realistic expectations for frequency and duration during recovery. For a detailed look at the range of support available, including personal care and skilled nursing, explore our caregiver services.
Hospital-to-home pathways can speed coordination of skilled care; Home Matters Caregiving can discuss these options and help arrange in-home visits through your discharge planner or community referrals.
How Does Skilled Nursing and Therapy at Home Aid Recovery?
Skilled nursing and home therapy tackle clinical needs and functional gaps in the patient’s living environment, which speeds recovery by practicing tasks where they matter most. Skilled nurses manage wound care, give medications or IV treatments, and monitor vitals so care happens safely at home. Physical therapists advance mobility with graded exercises and gait training; occupational therapists adapt tasks and suggest equipment so daily routines are achievable. Interventions set measurable goals — longer walking distance, less transfer assistance — and clinicians track progress to guide therapy frequency and discharge from services.
When therapists and nurses coordinate with physicians and caregivers, they close the loop between hospital protocols and real-world functioning, improving independence and long-term outcomes.
What Medication Management and Personal Care Services Are Available?
Medication management includes reconciliation, clearly labeled dosing, blister packaging, reminders, and in-home administration for complex regimens — all steps that reduce missed doses and adverse drug events. Personal care covers bathing, dressing, toileting, feeding, and companionship while the patient regains strength. Home-care staff and family caregivers watch for side effects and report changes to clinicians, serving as the first line of early detection. Combining medication management with personal care helps maintain adherence and daily safety without overloading family members.
Simple practices — daily medication checks or weekly blister packs — turn prescriptions into dependable routines that support recovery milestones.
Which Specialized Transitional Care Programs Are Available in Philadelphia?
Specialized transitional programs focus on condition-specific needs — orthopedic post-surgery pathways, cardiac transitional programs, and stroke recovery services — and are designed around typical recovery timelines and complication risks. These programs combine home-based therapy, nursing, and care coordination with condition-focused education for patients and caregivers to improve function. Orthopedic pathways stress mobility and fall prevention; cardiac programs closely monitor symptoms and meds; stroke programs focus on communication, mobility, and cognitive support. Many local programs work directly with hospital discharge teams to streamline referrals and first home visits.
Look for these condition-focused features when evaluating local options:
- Therapy protocols tailored to clinical milestones for the condition.
- Early home visits within 24–72 hours after discharge for higher-risk cases.
- Education and hands-on training for family caregivers on condition-specific care.
These features help ensure the hospital-to-home transition matches expected recovery paths and provides measurable checkpoints for progress.
How Is Post-Surgery and Stroke Recovery Supported at Home?
Post-surgery and stroke recovery at home rely on staged therapy, wound and medication monitoring, and stepwise goals that match the procedure or neurologic deficit. Orthopedic protocols focus on safe weight-bearing, gradual strengthening, and adaptive equipment to rebuild mobility while preventing falls. Stroke recovery emphasizes ADLs, speech or swallow therapy when needed, and cognitive strategies; therapists adapt exercises to the home to reinforce real-world gains. Families should watch for warning signs — fever, uncontrolled pain, sudden neurologic changes — and contact clinicians when they appear. Tracking progress against therapy goals helps determine when services can taper.
Coordinating nurses, therapists, and the primary physician creates a seamless path that reduces complications and supports realistic recovery timelines.
What Resources Exist for Dementia Care and Family Caregiver Respite?
Dementia-focused transitional support centers on safety planning, behavior-management strategies, and respite services to sustain long-term caregiving while preserving the person’s dignity. In-home caregivers trained in dementia care use routines, environmental cues, and de-escalation techniques to reduce agitation and maintain daily structure. Respite — short-term in-home or facility care — prevents caregiver burnout and helps maintain safer care over time. Family caregivers also benefit from support groups, training modules, and local community programs that offer practical guidance and emotional support; these resources complement clinical services by addressing the day-to-day challenges of dementia care.
Prioritizing safety planning, caregiver training, and scheduled respite helps families keep quality care at home while protecting caregiver health.
How Can Philadelphia Families Find and Choose the Right Home Care Agency?
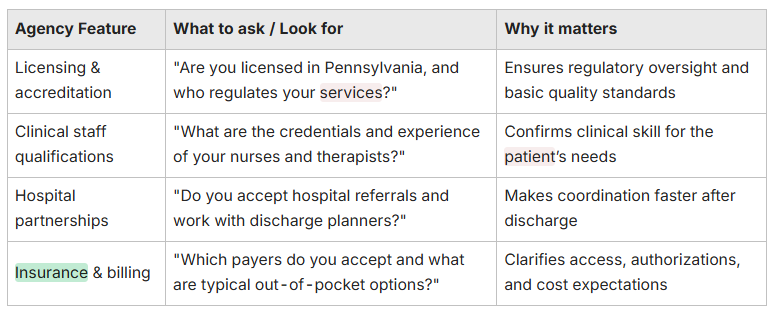
Choosing an agency means checking licensing, insurance acceptance, hospital relationships, clinical capabilities, and cultural fit so services match the patient’s needs and family preferences. Verify state licensure or certification, ask about staff credentials, confirm which payers they accept, and request examples of hospital partnerships or transitional programs. Expect transparency about service scope, emergency procedures, and communication methods. Structured interview questions let families compare providers objectively and pick the one with the right clinical mix and reliable scheduling. To understand our philosophy and commitment to quality care, you might find our Why Home Matters page and information about us insightful.
The table below turns agency features into practical questions families can ask during interviews.
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.


