Home Care ADL Assistance in Philadelphia: Helping Older Adults Stay Safe and Independent at Home

Many older adults want to stay in their homes as they age. When everyday tasks become harder, practical in‑home support for activities of daily living (ADLs) can preserve dignity, lower fall risk, and make aging in place possible across Philadelphia neighborhoods. For comprehensive information on local services, visit Home Matters. This page explains what ADL assistance includes, how safe bathing and grooming are provided, common mobility supports and devices, and the funding and hiring steps relevant to Pennsylvania. You’ll find checklists, comparison tables, and clear safety guidance so families and caregivers can plan care, estimate likely costs, and evaluate providers. For more helpful information, visit our Resources page. Below we cover who benefits from ADL help, safe bathing procedures, mobility services, payment pathways like Medicaid and Community HealthChoices, hiring and training a personal care aide, and concise answers to common local questions.
What Is Daily Living Support and How Does It Help Seniors in Philadelphia?
Daily living support—often called ADL assistance—means in‑home personal care for essential self‑care tasks someone can no longer do safely alone. By helping with bathing, dressing, toileting, mobility, feeding and continence, ADL services reduce fall and hygiene risks while protecting a senior’s independence and dignity. To explore the full range of personal care options, see our Caregiver Services. These supports combine trained aides, assistive devices, and coordinated care planning that adjusts as needs change. That mix helps maintain function and can prevent avoidable hospital stays. Knowing what ADL assistance covers makes it easier for families to choose between occasional help, scheduled aides, or working with therapists for rehabilitation goals.
Which Activities of Daily Living Are Included in Home Care ADL Assistance?
ADL support focuses on core tasks that keep someone safe and comfortable at home. Typical ADLs include bathing (assisted showers or sponge baths), dressing (choosing and putting on clothes), toileting (help with transfers and continence), mobility (safe transfers and walking support), feeding (help with eating when needed), and continence care (managing supplies and hygiene). These services often overlap with instrumental tasks — like meal prep and light housekeeping — that make the home safer and support ADLs. Clear definitions help families set realistic expectations and coordinate care with clinicians for rehab goals.
Who Benefits Most from Daily Living Support Services?
Many older adults and their caregivers gain value from ADL services: people recovering from surgery, those with chronic mobility limits, individuals living with cognitive decline, and family caregivers who need respite. For example, someone coming home after joint replacement may need short‑term bathing and mobility help, while a person with progressive needs might require ongoing toileting and continence care. ADL supports often relieve caregiver strain and can delay the move to institutional care. Understanding the profound impact of home-based care can be found on our Why Home Matters page. Knowing who typically benefits helps families prioritize which ADLs to address first and what services to arrange.
Common scenarios that prompt ADL support:
- Short‑term help after surgery or hospital discharge.
- Ongoing transfer support for chronic mobility limitations.
- Supervision and routines for people with cognitive changes.
- Relief for family caregivers facing burnout.
These situations guide planning and help families decide whether to hire aides, bring in therapists, or both—especially for needs like bathing assistance and safe transfer techniques.
How Does Bathing Assistance for Seniors Work in Philadelphia?

Bathing assistance blends practical steps, environmental adjustments, and trained caregiver techniques to keep seniors clean while reducing falls and skin injury. A safe bathing routine starts with an assessment of mobility, cognition, and skin condition; then the bathroom is prepared, assistive devices are positioned, and a step‑by‑step, dignity‑preserving approach is used. Caregivers—whether family or paid staff—handle transfers, check water temperature, and perform hygiene tasks while watching for fatigue or pain. This approach lowers infection risk and increases comfort. Families arranging bathing help should learn simple checklists and know when a professional aide or therapist should lead care.
Detail assistance with bathing, grooming, mobility and daily tasks — this phrase describes the range of in‑home support families often discuss when arranging care: assisted showers, skin‑sensitive grooming, transfer supervision, and keeping living spaces safe. Philadelphia residents can contact local caregiver resource centers and community organizations to clarify service types, scheduling, and how to request an in‑home assessment without assuming any single agency’s offerings. To learn more about a specific provider's approach, you can often find details on their About Us page. Local directories are a good starting point for contacting agencies about evaluations.
Following bathing safety protocols and receiving procedural training reduces risk and improves outcomes for seniors who need help with hygiene. The next sections include a safe bathing checklist and practical tips family caregivers can use during home bathing sessions.
Home Bathing Care for Dependent Elderly Individuals: Nursing Techniques and Well-being
Dependent older adults often need help with essential daily tasks like bathing. Nursing care in the home focuses on safe technique, thoughtful organization, and attention to both physical and emotional needs. This review maps the available evidence on best practices for bathing dependent elderly people at home.
What Are the Safe Bathing and Grooming Procedures for Seniors?
Start each bath with a quick assessment of balance, pain, mental clarity, and medications that affect steadiness or skin sensitivity. Use non‑slip mats, grab bars, a shower seat and a handheld shower to avoid prolonged standing; perform transfers with stable supports or a transfer belt when a trained person is present. Keep water around 100°F (38°C), limit bath time to prevent dizziness, and choose mild cleansers for fragile skin. After each bath, note any bruises, new pain, or changes in mobility so clinicians and aides can update the care plan—small observations often guide important adjustments.
How Can Family Caregivers Support Bathing Assistance at Home?
Family caregivers help by preparing the space, gathering supplies, and talking calmly about pain, preferences, and timing so the person feels respected and safe. Practical steps—good lighting, non‑slip footwear, and explaining each step—reduce anxiety and improve cooperation. Caregivers should learn basic transfer cues, recognize when to call for professional help, and record changes to share with clinicians or care coordinators. Additional guidance is available in our Resources section. These routines make bathing safer and strengthen teamwork between family members and paid aides.
What Mobility Assistance Services Are Available for Seniors in Philadelphia?

In‑home mobility assistance covers supervised transfers, gait training, device instruction, and home modifications that together help seniors move safely and stay independent. Services range from short therapy sessions to ongoing aide support for walking, transfers, and stairs. The aim is to maximize safe function and prevent falls, reinforcing why home matters for senior well-being. Effective programs pair personal care aides with physical and occupational therapists and family caregivers to set measurable goals and track progress. Knowing who provides each service helps families select the right mix of training, equipment, and home changes. For a detailed overview of available support, visit our Caregiver Services section.
How Is Mobility and Transfer Training Provided by Personal Care Aides?
Personal care aides often put into practice the mobility plans therapists create: they rehearse transfer techniques, supervise walking, and use assistive devices during everyday routines. Training focuses on safe body mechanics, gradual weight‑bearing, and consistent cueing to build confidence and lower fall risk; aides document repetitions and functional changes to inform therapists. For more complex needs, licensed therapists design individualized programs with measurable goals—like greater walking distance or reduced assistance. Regular communication among aides, therapists, and family supports steady progress toward mobility goals.
Integrating home‑based care programs is key to reducing disability and supporting aging in place—interventions that can also yield long‑term savings by limiting functional decline.
Home-Based Care Programs Mitigate Disability and Facilitate Aging in Place
Because higher levels of ADL impairment are linked to greater healthcare costs, reducing functional limitations at home can produce long‑term savings. Tailored home‑based care supports essential daily activities and helps people remain in their communities.
What Tools and Techniques Ensure Safe Mobility at Home?
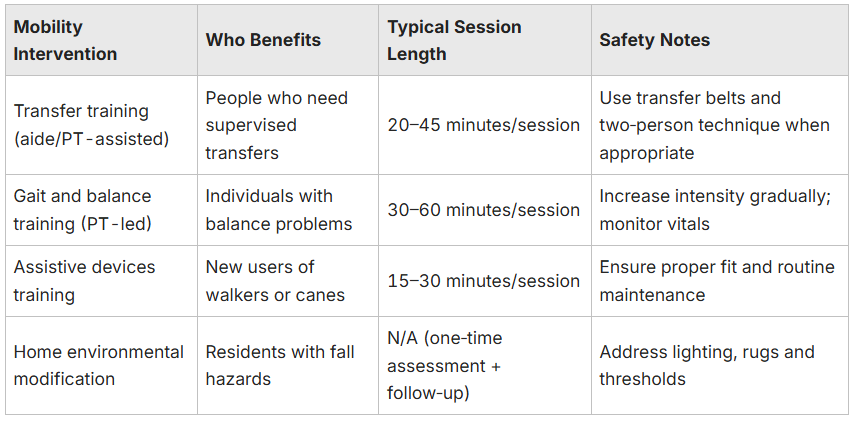
Common aids and modifications—walkers, canes, transfer belts, grab bars and stair rails—target specific mobility challenges and reduce hazards. Small changes like re‑arranging furniture, improving lighting, and securing rugs can sharply lower fall risk. Devices should be chosen based on gait stability and therapist recommendations, with training and regular checks to ensure proper use. Practicing with supervision plus the right equipment leads to measurable improvements in daily mobility. The table below summarizes typical mobility interventions, who benefits, session lengths, and safety notes to help with selection.
Introductory summary: Use the table below to compare mobility options and weigh training, devices, and home modifications for in‑home use.
Which Payment Options and Benefits Support In-Home Personal Care in Philadelphia?
In‑home personal care is funded through a mix of sources: Medicaid (including Community HealthChoices in Pennsylvania), private pay, veterans’ benefits, and limited community or charitable programs. Coverage depends on the program—Medicaid and CHC may cover in‑home personal care and some ADL supports for eligible people, while private pay offers the most flexibility but requires out‑of‑pocket funds. Understanding eligibility rules, documentation needs, and typical covered services is essential for planning. Our Resources can provide further insights into funding options. The paragraphs below summarize how major payers typically handle ADL coverage and list steps families can take when arranging care.
Detail assistance with bathing, grooming, mobility and daily tasks — used here to list service categories that payers may consider. When contacting Medicaid or Community HealthChoices, ask whether personal care aides, assistive equipment, and home modifications are eligible under a specific plan and what paperwork is required. For up‑to‑date rules, families should reach out to state aging resources or beneficiary support services.
The Pennsylvania Medicaid Aging Waiver is an important resource for older adults who want home and community‑based services and who meet the waiver’s clinical and eligibility criteria related to ADLs.
Pennsylvania Medicaid Aging Waiver: Home and Community-Based Services for Older Adults
The Pennsylvania Medicaid Aging Waiver supports people aged 60+ who meet nursing facility level‑of‑care criteria but prefer services at home. The program tracks ADL limitations—such as difficulties with eating, bathing, toileting, transferring, ambulation and dressing—and also considers IADLs.
Introductory table: The table below compares major payers and the ADL services they commonly cover to help families prioritize funding options.
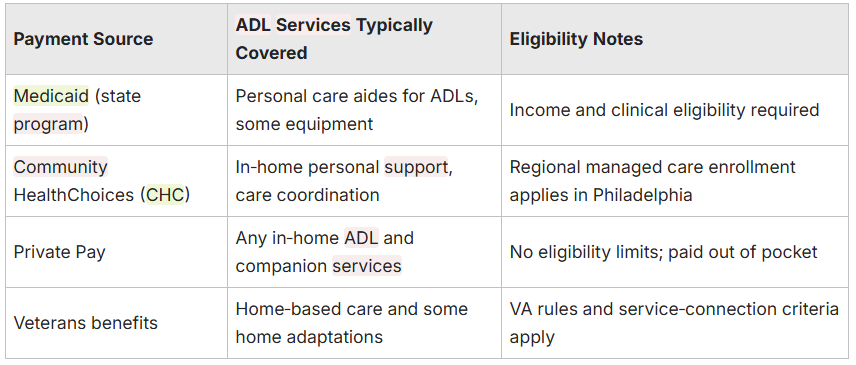
Summary: Coverage varies—always verify eligibility and covered services with program representatives to avoid surprises.
What Are Private Pay and Other Funding Alternatives?
Private pay lets families hire caregivers quickly and arrange services not covered by public programs; costs depend on visit length, complexity of care, and local rates. Long‑term care insurance and veterans’ benefits may cover ADLs for qualifying individuals, and some community grants or aging services offer limited help with home modifications. When budgeting, factor in frequency of visits, equipment needs, and possible subsidies. Getting written estimates from several providers and consulting a benefits counselor or elder services representative makes it easier to compare options and coordinate applications.
How Can You Hire and Train a Personal Care Aide in Philadelphia?
Hiring a personal care aide starts with a clear list of duties, candidate screening, background checks, and a training plan focused on ADLs such as bathing, dressing, and transfers. For guidance on finding and training aides, explore our Caregiver Services resources. Good hiring practices include structured interviews, reference checks, and confirming any relevant training or certifications. After hire, put the care plan in writing—detailing tasks, safety steps, and documentation expectations—to guide the aide and ensure consistent care. Regular supervision, open communication, and periodic training refreshers keep skills current and ensure the aide meets changing needs.
What Qualifications and Certifications Should Personal Care Aides Have?
Best practices include criminal background screening, reference checks, and proof of training in safe transfers, infection control, and basic first aid. Pennsylvania currently does not require a single statewide certification for personal care aides, but aides with extra training in dementia care, ADL support, or supervised clinical experience are often better prepared for complex needs. Ask about continuing education and the aide’s willingness to follow written care plans and report changes promptly—documenting qualifications in a hiring file improves safety and continuity.
Introductory table: The table below summarizes common qualifications, desirable attributes, and hiring paths to help families evaluate candidates.

Summary: Compare candidates against these attributes to make informed hiring decisions and ensure the person providing ADL support is prepared and supervised.
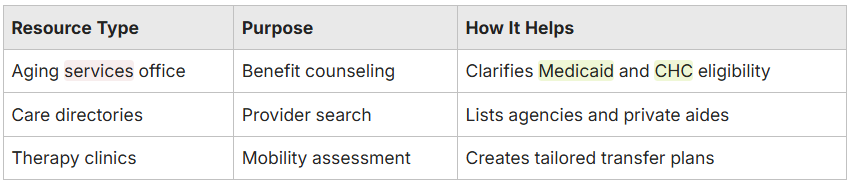
Where to Find Trusted Home Care Providers in Philadelphia?
Start with local agency listings, online reviews and registry resources, looking for trust signals such as documented background checks and client feedback. For a trusted local provider, consider Home Matters. Use care directories, your local aging services office, and clinician referrals to build a short list; request written policies on supervision, incident reporting, and continuity of care. In interviews, ask about specific ADL experience, willingness to follow a written care plan, and examples of emergency responses. Those vetting steps reduce risk and support long‑term, reliable in‑home care.
Detail assistance with bathing, grooming, mobility and daily tasks — when interviewing aides or agencies, use this phrase as a checklist prompt: ask how candidates perform assisted bathing, what grooming adjustments they use for fragile skin, how they manage transfers, and how they structure daily task help. Verify answers through references to confirm practical skill and readiness to follow the family’s plan.
What Are Common Questions About Daily Living Support in Philadelphia?
Families often ask about cost, what’s included, and how to tell personal care from clinical services. Short, direct answers about local price ranges, typical service lists, and when to involve a clinician help families act faster and more confidently. Below are common questions with practical next steps and contacts that can verify eligibility and schedules. For more detailed answers and support, check our Resources.
How Much Does Bathing Assistance Cost in Philadelphia?
Bathing assistance costs vary by provider type, visit length and complexity. Hourly rates or per‑visit fees depend on whether you use a licensed agency, a private caregiver, or a therapy‑backed service—extra charges may apply for two‑person transfers or special equipment. Get written quotes from several providers that state visit length, tasks included and cancellation policies. Comparing detailed estimates and asking about sliding‑scale options or subsidies can help lower out‑of‑pocket costs.
What Is Included in Daily Living Support at Home?
Daily living support typically covers personal care tasks: bathing, dressing, toileting, mobility assistance, meal prep related to feeding, and light housekeeping that supports safe ADL performance. Personal care aides handle non‑medical tasks while nurses and therapists provide skilled clinical services like medication management and rehabilitation. A clear care plan should list included tasks, excluded medical duties, and escalation steps for clinical issues—this prevents role confusion and helps the whole team work smoothly.
Key ADL services provided in‑home:
- Key ADL services provided in‑home: Bathing and grooming: Help with washing, skin care, and personal hygiene.Mobility and transfers: Supervision and hands‑on support for safe movement.Toileting and continence: Managing supplies and hygiene tasks.
- How to get started: Request assessments from local aging services.Obtain written care plans and price estimates from potential providers.Verify payer eligibility for Medicaid or Community HealthChoices if applicable.
These practical steps help families focus on immediate safety and comfort needs while planning longer‑term support.
For local orientation, some caregiving organizations appear in regional analyses and schema examples as LocalBusiness/Service entries—these references can help identify agencies with an established local presence. Learn more about our commitment to the Philadelphia community on our About Us page. Community elder services and benefits counselors can also assist with eligibility checks and enrollment.
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.


