In-Home Alzheimer's and Dementia Care in Philadelphia: How Specialized Caregivers Support Your Loved One

Alzheimer's and other dementias change everyday life in ways that need focused, compassionate care. This guide explains how in-home memory care in Philadelphia helps keep people safe, preserve dignity, and maintain meaningful routines. You’ll read what specialized memory care looks like, which services to expect, how trained caregivers use evidence-based methods, and practical steps to find local respite and support. We also outline cost factors and how to compare pricing and funding options in the Philadelphia area. Throughout, we point to local resources and vetting tips so families can make clear, informed choices about home-based dementia care. Our aim is simple: give families practical information and show how Home Matters’ specialized approach supports real needs at home.
What Is Specialized Alzheimer's and Dementia Care in Philadelphia?
Specialized Alzheimer's and dementia care at home combines dementia-focused training, predictable routines, and behavior strategies to keep people safer and more engaged where they live. Caregivers use dementia-aware communication, adjust the environment, and design daily rhythms around each person’s abilities to reduce confusion and distress. The outcome is steadier daily function, fewer safety incidents, and a better quality of life. In Philadelphia, this approach also links families with local supports — memory clinics, caregiver groups, and community programs — so care plans reflect neighborhood resources and cultural preferences. Below are three clear benefits families commonly see when a specialized approach is in place.
This section highlights three immediate benefits:
- Consistent routines reduce anxiety: Predictable schedules help orient memory and often lower agitation.
- Tailored communication improves cooperation: Dementia-specific cues and simple language increase participation in daily tasks.
- Safety-focused adaptations lower risk: Home modifications and attentive supervision reduce falls and medication mistakes.
These benefits flow directly from how dementia changes daily life and lead into a closer look at the functional shifts families typically notice.
How Do Alzheimer's and Dementia Affect Daily Life?
Alzheimer's and related dementias gradually affect memory, planning, and practical skills — the tasks we take for granted like dressing, cooking, and handling money. In early stages people often have short-term memory gaps and trouble with complex tasks; later stages bring more confusion, mobility challenges, and increasing need for help with basic activities of daily living (ADLs). These changes can create safety risks such as wandering, missed medications, and poor nutrition, which is why proactive care planning matters. Knowing how decline usually progresses helps families and caregivers simplify tasks, set up helpful routines, and introduce tools that support independence as long as possible. That understanding makes it easier to choose the right services and caregiver training as needs change.
What Services Are Included in Specialized Memory Care?

In-home memory care bundles services that target safety, daily functioning, and cognitive support and are tailored to each person’s stage of dementia. Providers typically combine companionship, personal care, medication oversight, behavioral support, and individualized care planning to build consistent, person-centered days. The table below summarizes common service categories, what they do, and what families can expect from each.
Services commonly included in in-home memory care:
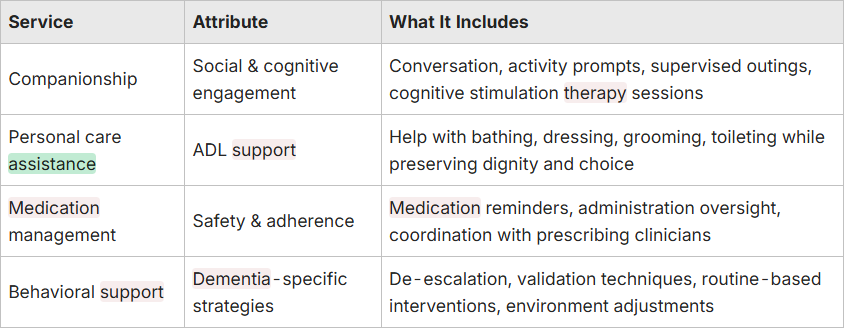
Families should expect a clear, written care plan, regular updates as needs change, and service adjustments as the condition progresses. A structured list like this also makes it easier to compare providers and confirm essential elements — for example, medication oversight and mobility support — are included. For a detailed look at specific offerings, you might explore a provider's caregiver services page.
How Do Specialized Caregivers Support Loved Ones with Alzheimer's and Dementia?
Specialized caregivers help by creating predictable days, monitoring safety, and using communication methods that lower confusion and distress. They deliver person-centered care: matching activities to current abilities, using visual cues, and gently redirecting when behaviors arise. Caregivers also work with families and local clinicians to notice changes and update the plan, keeping care consistent with medical advice. Below are practical actions caregivers take that often improve daily functioning and emotional well-being.
Common caregiver actions include:
- Establishing consistent routines: Regular schedules reduce sundowning and help orientation.
- Using clear communication techniques: Short sentences, calm redirection, and validation help maintain cooperation.
- Implementing safety protocols: Supervision strategies and environmental tweaks reduce hazards and medication errors.
These roles require specific dementia training and ongoing supervision — which brings us to the types of training and techniques caregivers use.
What Training and Techniques Do Dementia Caregivers Use?
Dementia caregivers train in focused communication, behavior de-escalation, and models that explain how abilities change over time. Common topics include validation therapy, breaking tasks into steps, the GEMS model for understanding behavior, and cognitive stimulation techniques to encourage engagement. On-the-ground methods include visual cueing, simplifying multi-step tasks, using music and reminiscence to connect emotionally, and gentle redirection to ease agitation. Continuous education and supervised case reviews help caregivers use these practices consistently and adapt them as symptoms evolve. Knowing these skills helps families vet providers for dementia-specific competence rather than general home help.
Evidence-Based Training for Caregivers Supporting Individuals with Dementia
Behavioral skills training is an evidence-based method to build caregiver competence when supporting people with intellectual and developmental disabilities, and early work suggests similar approaches can improve caregiver performance in dementia care. Research on long-term skill retention and the direct link between caregiver training and client outcomes is still growing, but initial findings are promising and point to cost-effective alternatives to traditional training programs.
Review of evidence-based approaches to caregiver training, 2019
How Do Caregivers Promote Dignity and Independence at Home?
Caregivers protect dignity and encourage independence by offering meaningful choices, simplifying tasks, and using adaptive tools that match abilities. Simple tactics — offering two choices instead of open questions, using adaptive clothing or utensils, and breaking tasks into small steps — let people do as much as they can and keep a sense of control. Respectful language, honoring routines and personal preferences, and focusing on strengths more than limitations help preserve self-worth and reduce resistance. Small environmental changes — better lighting, clear labels, or uncluttered paths — support function without feeling intrusive. These dignity-first strategies ease stress for both the person with dementia and their family.
What Are the Benefits of In-Home Dementia Care in Philadelphia?
In-home dementia care keeps people in familiar surroundings and routines, which lowers confusion and stress while preserving neighborhood ties and cultural habits. One-on-one support at home allows highly personalized care, flexible schedules, and direct family involvement — all of which help day-to-day functioning and emotional comfort. Compared with moving into an unfamiliar facility, staying at home often reduces anxiety and behavioral incidents and supports nutrition and hygiene by keeping trusted patterns. Below are common, evidence-backed advantages families report when they choose in-home memory care.
Key benefits include:
- Familiar environment reduces distress: Home-centered care keeps the cues that help memory and orientation.
- Personalized attention supports function: One-on-one care adapts activities to abilities and life preferences.
- Stronger family collaboration: Care plans integrate family knowledge and encourage consistent support.
These benefits often show up as fewer emergency visits and better quality-of-life measures — topics families can discuss with local memory centers like the Penn Memory Center or advocacy groups such as the Alzheimer's Association (Delaware Valley Chapter).
How Does In-Home Care Improve Quality of Life for Seniors?
In-home care protects daily rituals, supports meaningful activity, and removes environmental triggers that can cause confusion or agitation. Personalized elements — favorite music, framed photos, and routine-based tasks — boost mood and give continuity that helps counter disorientation. Regular supervision and medication adherence reduce risks of hospitalization and medication errors, while tailored nutrition and hygiene support preserve physical health. Together, these changes create more comfortable days, reduce caregiver strain, and lead to fewer crisis-driven transitions. Clinical guidance and memory care research consistently point to familiarity and routine as key drivers of these improvements.
Cognitive Stimulation Therapy for Dementia: Enhancing Cognition and Quality of Life
Aims: To evaluate whether Cognitive Stimulation Therapy (CST) improves cognition and quality of life for older adults with dementia. Method: A single-blind, multi-centre randomized controlled trial with 201 older adults diagnosed with dementia assessed changes in cognitive function and quality of life. Results: At follow-up, participants in the CST group showed statistically significant improvements on the Mini-Mental State Examination (P=0.044), the ADAS–Cog (P=0.014), and the Quality of Life – Alzheimer's Disease scale (P=0.028) compared with controls.
Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial, 2003

Family members bring the personal history, preferences, and emotional context that make person-centered plans work. Regular updates, shared care notes, and scheduled planning meetings keep everyone aligned with caregivers and clinicians. When families are true partners, transitions and changes in behavior are handled more smoothly, and caregivers can use familiar cues that resonate with the person’s life story. At the same time, clear roles and boundaries protect caregiver well-being and keep support sustainable. Thoughtful family involvement links home-based services with clinical resources and community programs.
How Can Families Access Dementia Caregiver Support and Respite Services in Philadelphia?
Finding caregiver support and respite in Philadelphia starts with locating local organizations, comparing service types, and arranging the kind of relief that fits your schedule. Map nearby resources — memory clinics, caregiver support groups, and county aging services — then evaluate respite formats like hourly in-home help, overnight coverage, or adult day programs. Check eligibility for subsidized programs through state agencies and coordinate with your clinical team so respite matches medical and behavioral needs. The short steps below show how to secure support quickly and responsibly in a local context.
Families can begin with three practical steps:
- Identify local resources: Reach out to memory centers, the Alzheimer's Association (Delaware Valley Chapter), and your county aging services to learn about programs.
- Vet respite formats: Compare hourly in-home respite, adult day programs, and overnight stays for safety and fit.
- Plan logistics: Arrange trial visits, review caregiver training and credentials, and prepare a brief care summary for respite workers.
Following these steps helps families get the support they need with less friction — and gives caregivers necessary breaks to stay healthy and effective.
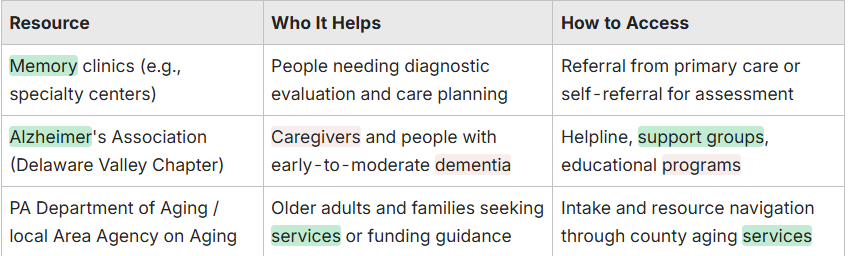
What Local Resources and Support Groups Are Available?
Philadelphia families have access to clinical, advocacy, and government resources that offer education, support groups, and referrals for in-home memory care and respite. Key resources include memory clinics connected to academic centers, the Alzheimer's Association (Delaware Valley Chapter) for support and education, and the PA Department of Aging or local Area Agency on Aging for navigation and funding help. Community caregiver groups and faith-based programs often run peer support and practical workshops. Additionally, many providers like Home Matters Caregiving offer their own online resources and guides for families. The table below maps common resource types, who they help, and how families typically reach them.
How Does Respite Care Help Family Caregivers?
Respite care gives caregivers planned breaks to rest, handle appointments, or recharge — available as short hourly visits or longer scheduled shifts. Benefits include reduced burnout, better mental health, and greater capacity to keep providing safe care at home. Respite also helps families stay employed and socially connected while ensuring the person with dementia has trained supervision and meaningful engagement. Planning for respite with trial sessions, clear care notes, and gradual handoffs eases transitions for the person receiving care. Coordinating respite with local agencies and clinical teams supports continuity and safety during caregiver breaks.
What Is the Cost of In-Home Memory Care in Philadelphia?
Costs for in-home memory care in Philadelphia vary by service model — hourly care, flat overnight shifts, or 24-hour/live-in support — and rise with specialized dementia training or higher clinical needs. Local labor markets, night shifts, and emergency coverage also affect prices. Families should collect multiple, itemized quotes that list included services, caregiver training, and supervision so they can compare value rather than price alone. Below are the main factors that typically drive cost estimates.
Factors that drive cost:
- Hours of care per week: More hours and overnight coverage increase total costs.
- Specialized training and supervision: Dementia-certified staff or clinical oversight usually raises rates.
- Level of clinical needs: High-acuity care, behavioral interventions, or mobility assistance affect pricing.
Knowing these factors helps families estimate budgets and shape conversations with providers and payers.
How Are Dementia Care Services Priced in Philadelphia?
Providers commonly bill hourly for daytime care, charge flat rates for overnight shifts, and set premium fees for 24-hour live-in coverage; specialized dementia training or higher caregiver-to-client ratios usually cost more. Typical ranges below give families a realistic starting point when requesting detailed quotes that specify tasks like medication oversight, ADL assistance, and behavior strategies. When comparing providers, ask whether dementia frameworks like GEMS or cognitive stimulation therapy are part of training and whether visits are clinically supervised. Clear, transparent quotes that tie fees to services and training help families evaluate cost-effectiveness and align care with needs.
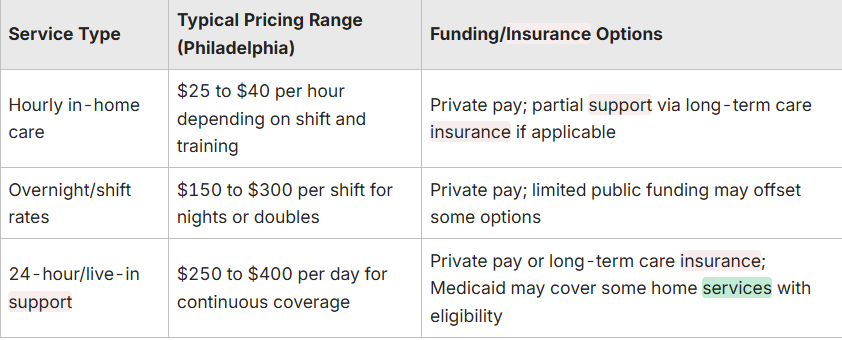
Ask providers for itemized estimates and inquire about sliding-scale options or bundled packages to understand likely monthly costs.
What Financial Assistance and Insurance Options Exist?
Several payers may help offset in-home memory care costs: Medicaid programs that fund home- and community-based services, VA benefits for eligible veterans, and private long-term care insurance where applicable. Eligibility rules and benefits vary, so contact your county aging services or a benefits counselor to explore options and start applications. Local agencies can identify waiver programs or state-funded respite supports for qualifying households. Engaging a social worker or case manager early in the process helps uncover potential funding pathways and prepares the paperwork you’ll need.
Why Choose Home Matters Caregiving for Alzheimer's and Dementia Care in Philadelphia?
Home Matters Caregiving is presented here as a local example of how specialized in-home Alzheimer’s and dementia care can be structured. To learn more about our mission and values, visit our website. A strong provider model blends dementia-focused caregiver training, individualized care plans, regular family communication, and coordination with community resources. When evaluating providers, look for evidence of dementia-specific training, clear care plans, and systems for family updates and clinical coordination. Presenting Home Matters as a model gives families a practical reference point to compare services across Philadelphia while avoiding exclusive endorsement.
What Makes Home Matters Caregiving’s Approach Unique?
A specialized dementia-care model emphasizes structured training, person-centered plans, and predictable communication that keeps families involved and informed. To understand why families choose Home Matters Caregiving, helpful differentiators include named frameworks used in training (for example, GEMS), routine-based activity programming, and formal behavior-management protocols. Concrete practices to look for are pre-visit care summaries, scheduled family check-ins, and caregiver mentorship focused on dementia techniques. When a provider spells out these elements, families can feel more confident they’re choosing services that will meet changing needs.
How Do Client Testimonials Reflect Care Quality?
Verified client feedback typically highlights reliability, respectful treatment, and steadier daily routines rather than broad promotional claims. Families often say that consistent caregivers who know personal histories reduce behavioral incidents and improve meal and hygiene routines. When checking credibility, prioritize documented reviews, specific outcome stories (for example, better sleep or fewer hospital visits), and references that confirm continuity of care. This kind of evidence helps families separate dementia-informed providers from general home-help services.
Frequently Asked Questions
What should families consider when choosing a caregiver for dementia care?
Prioritize experience and dementia-specific training. Ask how the caregiver communicates with someone experiencing cognitive decline, how they build personalized care plans that respect routines and preferences, and how they handle behavior changes. Check references and recent reviews to confirm reliability, and confirm the caregiver’s availability and flexibility to meet your schedule.
How can families ensure safety in the home for someone with dementia?
Start with a safety check: remove trip hazards, secure sharp objects, and reduce clutter. Add grab bars in the bathroom, improve lighting, and consider locks or alarms if wandering is a risk. Keep medications organized and emergency contacts visible. A caregiver trained in dementia-aware safety practices can further reduce risks and adapt the home as needs change.
What role does technology play in supporting dementia care at home?
Technology can boost safety, connection, and engagement. GPS devices and door alarms help monitor wandering risks; medication reminder systems improve adherence; and video calls make regular check-ins easier. Cognitive-stimulation apps and simple digital games can support mental engagement. Thoughtful use of technology complements hands-on care and can make daily routines safer and more predictable.
How can families manage caregiver stress while providing dementia care?
Protecting caregiver health is essential. Schedule regular breaks and use respite care when needed. Join support groups for practical tips and emotional support, divide tasks among family members, and set realistic expectations. Make time for stress-relief activities like walking, hobbies, or brief mindfulness practices. Open communication about responsibilities and feelings helps keep care sustainable.
What are the signs that a loved one may need more intensive care?
Warning signs include more frequent or severe confusion, trouble completing daily tasks, increased wandering, significant weight loss, or poor personal hygiene. If safety becomes hard to maintain or behaviors escalate beyond what current supports handle, it’s time to consider more comprehensive care. Regular professional assessments can guide those decisions.
How can families effectively communicate with a loved one with dementia?
Use clear, simple language and a calm tone. Speak slowly, give one instruction at a time, and allow time to respond. Nonverbal cues — a reassuring touch, eye contact, or gestures — often help. Validate feelings, avoid arguing about facts, and offer limited choices to preserve independence. Familiar settings and routines make conversations easier and more meaningful.


