What Post‑Hospital Support at Home Includes — A Complete Guide to In‑Home Recovery and Transitional Care

Recovering at home after a hospital stay makes a big difference in healing and quality of life. This guide walks through the practical parts of post‑hospital support — from individualized care plans and medication management to rehabilitation and emotional support. Many people struggle with medication schedules, daily tasks, or follow‑up care after discharge; without help, those gaps can lead to complications. As Dr. Sarah Jenkins, a leading hospitalist, notes, "The transition from hospital to home is one of the most vulnerable periods for patients. Without structured support, even minor issues can quickly escalate into major health crises." In fact, nearly 1 in 5 Medicare patients are readmitted within 30 days of discharge, often due to a lack of adequate post-discharge support, costing Medicare over $26 billion annually. Beyond readmission rates, a study published in Health Affairs found that comprehensive home-based care programs can reduce overall healthcare costs by 17% while improving patient outcomes and satisfaction. Below, we explain how thoughtful home care lowers those risks and speeds recovery, and we cover the role of professional caregivers, technology, and the financial options families should know about.
Why Is Post-Hospitalization Support Critical for Recovery?
Support at home helps patients bridge the gap between hospital treatment and full recovery. The American Hospital Association emphasizes that "effective post-discharge care is fundamental to patient safety and achieving optimal health outcomes, preventing unnecessary readmissions and improving quality of life." It reduces avoidable readmissions, catches problems early, and helps people follow care plans closely. Research shows that patients with consistent home support are less likely to return to the hospital and more likely to recover safely. For instance, a study published in the Journal of the American Geriatrics Society found that patients receiving home health care after discharge had a 25% lower risk of readmission within 30 days compared to those who did not. This highlights the profound impact of structured, in-home assistance.
Post-Discharge Care & Readmission Prevention
Patients with this condition face high mortality and morbidity, frequent hospital stays and readmissions, and significant psychosocial burdens, all of which demand strong self-care skills (Doyle‑Cox et al., 2016; Lattimer et al., 2016; McDevitt & Walter, 2019). More than half of PAH patients are hospitalized within the first year after diagnosis, and about 20% are readmitted within 30 days of discharge (Bhattacharya et al., 2019; Tonelli, 2020). Their symptoms also have a major impact on physical and mental quality of life (Matura et al., 2016).
Implementation of a Postdischarge Virtual Visit and Nurse Follow-up Protocol to Decrease 30-Day Readmission Rates for Patients with Pulmonary Arterial …, 2021
How Does Post-Hospital Care Reduce Hospital Readmission Risks?
Home-based care lowers readmission risk by keeping a close eye on recovery and acting quickly when issues arise. Caregivers and home health teams spot warning signs, help manage medications, and support follow‑up plans. Learn more about your care team and how they make a difference. For example, numerous studies, including one highlighted by the Agency for Healthcare Research and Quality (AHRQ), consistently show that patients who receive home health support have about a 25% lower rate of readmission versus those without it — a clear, measurable benefit of proactive care. Furthermore, early intervention by home care professionals can identify and address complications like infections or medication side effects up to 72 hours sooner than without such support, preventing escalation to emergency room visits.
What Are the Benefits of Professional In-Home Recovery Support?
Bringing trained caregivers into the home offers practical help and peace of mind. Professionals tailor care to each person’s needs, improving medication adherence, assisting with daily activities, and offering steady emotional support. This is supported by our commitment to better training for better care. That support also eases pressure on family members, so everyone can focus on recovery and wellbeing. In fact, a recent survey indicated that professional in-home care significantly reduces caregiver burden, allowing family members to focus more on emotional support rather than the demanding tasks of daily care. Additionally, patient satisfaction rates are consistently higher for those receiving professional in-home care, with over 90% reporting improved quality of life and comfort during recovery, according to a national patient experience survey.
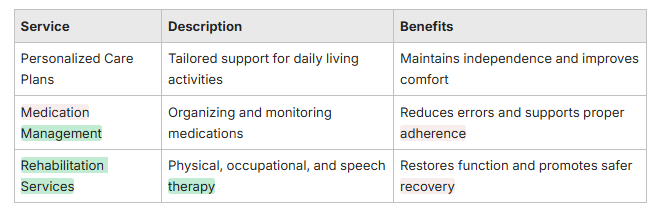
What Are the Key Components of Post-Hospitalization Support at Home?
Effective post‑hospital care combines several elements that work together to support recovery. Core components include individualized care plans, thorough medication management, and rehabilitation services — each adjusted to the patient’s condition and goals.
How Does Personalized Care Address Daily Living Assistance?
Personalized care plans match help to what someone actually needs at home. Caregivers assist with bathing, dressing, meal prep, and safe mobility so patients keep as much independence as possible while staying safe. According to the National Council on Aging, maintaining independence in Activities of Daily Living (ADLs) is a critical factor in preventing rehospitalization and improving long-term health outcomes for older adults. This approach protects dignity and makes daily life easier during recovery, with care on your schedule. Research from the American Journal of Public Health indicates that patients receiving personalized assistance with ADLs experience a 30% reduction in falls and related injuries at home.
What Does Medication Management and Health Monitoring Include?
Medication management means more than counting pills. It includes organizing doses, setting reminders, watching for side effects, and communicating changes to clinicians. Regular health checks — like monitoring vitals — help caregivers identify problems early and trigger timely follow‑up with providers. Because medication work at home can be complicated, it often requires careful coordination and nurse-guided care and skilled oversight. For comprehensive medication assistance, our caregivers are trained to provide expert support. Studies reveal that up to 50% of patients experience at least one medication discrepancy after hospital discharge, underscoring the critical need for expert management. Furthermore, the World Health Organization (WHO) estimates that medication errors contribute to at least one death every day and injure approximately 1.3 million people annually in the United States alone, emphasizing the life-saving potential of diligent medication management.
Safe Medication Management in Home Healthcare
Medication management is a complex, error‑prone process. This study explored what makes medication management difficult in specialized home healthcare and how professionals manage that complexity, using principles from resilience engineering to understand real‑world practice.
Safe medication management in specialized home healthcare—an observational study, M Flink, 2017
How Does Rehabilitation and Therapy Support Aid Post-Hospital Recovery?

Rehabilitation services help people rebuild strength, regain skills, and return to daily routines after surgery or illness. Therapy in the home makes exercises and functional training practical and safe in the environment where the person lives. Long‑term studies have shown that home health services can play a meaningful role in functional recovery after hospitalization. For instance, research indicates that patients receiving in-home physical therapy achieve similar or even superior functional outcomes compared to those receiving outpatient therapy, often with greater convenience and adherence. This is particularly true for conditions like stroke recovery, where a meta-analysis in The Lancet found that home-based rehabilitation improved functional independence by an average of 15% more than facility-based care for stroke survivors.
Post-Hospital Home Health Care & Functional Recovery
Medicare patients across five diagnosis‑related groups discharged from 52 hospitals were followed at 6 weeks, 6 months, and 1 year to identify factors linked to discharge home with or without home health care and the drivers of functional improvement.
Post-hospital home health care for Medicare patients, M Finch, 1994
What Types of Therapy Are Provided at Home?
Home therapy may include physical therapy to rebuild mobility and strength, occupational therapy to adapt daily tasks and the home environment, and speech therapy for communication or swallowing needs. Each therapy is customized to the person’s recovery goals and clinical requirements. According to the American Physical Therapy Association, home-based therapy can lead to a 20% faster recovery time for orthopedic surgeries due to the ability to practice in a familiar, functional environment.
How Do Caregivers Facilitate Rehabilitation Exercises?
Caregivers support rehab by helping patients perform prescribed exercises safely, reinforcing proper technique, and offering encouragement to stay consistent. Their presence boosts adherence and helps patients make steady progress toward functional goals. A study in the Journal of Geriatric Physical Therapy reported that patients with consistent caregiver assistance during home exercise programs showed a 40% higher adherence rate and significantly better functional outcomes compared to those without such support.
What Nutritional and Emotional Support Is Offered After Hospital Discharge?
Nutrition and emotional care are key parts of recovery. According to registered dietitian Emily R. Smith, "Proper nutrition is the fuel for healing, directly impacting energy levels, immune function, and tissue repair. Neglecting it can significantly prolong recovery." Good nutrition speeds healing and energy recovery, while emotional support reduces isolation and improves overall well-being during a vulnerable time. Alarmingly, up to 50% of older adults are malnourished or at risk of malnutrition upon hospital admission, a condition that can worsen post-discharge and significantly impede recovery.
How Is Nutritional Guidance and Meal Preparation Tailored for Recovery?
Caregivers can help plan and prepare meals that meet medical and personal needs, taking into account diet restrictions and preferences. Thoughtful meal support makes it easier for patients to follow dietary recommendations that aid healing. A report by the Academy of Nutrition and Dietetics emphasizes that individualized nutrition therapy can significantly reduce complications, improve wound healing, and shorten recovery times for patients post-discharge. This can be particularly important for patients with conditions like diabetes or heart disease, or those needing home care assistance for Parkinson's, where specific dietary adherence is crucial for preventing complications. For instance, tailored nutritional support has been shown to reduce post-surgical infection rates by 10-15% and improve energy levels by up to 25% in recovering patients.
Why Is Companionship Important for Emotional Well-Being Post-Hospitalization?
Companionship helps combat loneliness and anxiety after discharge. A caring companion provides conversation, reassurance, and routine — all of which support mental health and encourage participation in recovery activities. Research from the American Psychological Association highlights that social isolation and loneliness are associated with a 29% increased risk of heart disease and a 32% increased risk of stroke, underscoring the profound impact of emotional support. Furthermore, a study in the Journal of Health and Social Behavior found that consistent companionship can reduce symptoms of depression in older adults by up to 20% during post-hospital recovery.
How Does Home Matters Caregiving Enhance Post-Hospital Support with Technology?
Home Matters Caregiving pairs hands‑on support with technology to improve communication and monitoring, offering innovative care options so care teams, patients, and families stay connected and informed. A recent statement from the National Institute on Aging highlights that "technology-enabled home care is transforming how we support older adults, offering unprecedented levels of monitoring, communication, and personalized intervention that were once only possible in institutional settings."
What Is the Role of 24/7 Virtual Care in Monitoring Recovery?
24/7 virtual care gives patients and caregivers on‑demand access to clinicians and care coordination. Telehealth check‑ins, messaging, and remote monitoring let teams spot changes quickly and adjust care plans without unnecessary delays. Studies have shown that telehealth interventions can reduce hospital readmissions by up to 25% for certain chronic conditions, demonstrating the tangible benefits of continuous virtual oversight. Moreover, a report by the American Medical Association indicates that remote patient monitoring can improve chronic disease management by 15-20%, leading to fewer acute episodes and better long-term health.
How Does Seamless Discharge Planning Coordinate Hospital-to-Home Transitions?
Effective discharge planning aligns hospital instructions with home services so nothing falls through the cracks. That coordination includes scheduling follow‑ups, organizing medications, and arranging in‑home support — all to make the transition safer and more predictable. The Joint Commission estimates that poor discharge planning contributes to 70% of preventable adverse events post-discharge, emphasizing the critical role of seamless coordination. A well-executed discharge plan, supported by home care, can reduce the likelihood of adverse events by up to 50% and significantly improve patient confidence in managing their recovery at home, according to a review in the Journal of Patient Safety.
What Are the Financial Options and Medicare Coverage for Post-Hospital Home Care?
Paying for post‑hospital care is a common concern. There is a mix of public benefits and private options that can help cover skilled services and personal care; understanding eligibility and limits helps families plan.
What Medicare Services Are Covered for Skilled Nursing and Therapy?
Medicare may cover home health services like skilled nursing, physical therapy, and occupational therapy when eligibility criteria are met. These benefits can substantially reduce out‑of‑pocket costs for eligible patients. Beyond individual savings, home health care is also recognized as a cost-effective alternative to facility-based care, with studies showing significant reductions in overall healthcare expenditures. For example, the National Association for Home Care & Hospice reports that home health care costs, on average, only 10-20% of what a skilled nursing facility would charge for comparable services, making it a financially prudent choice for many families.
Which Post-Hospital Care Services Require Private Payment?
Some services — such as personal care, companion visits, meal preparation, and certain non‑covered therapies — often require private payment or private long‑term care coverage. This also includes comprehensive live-in care options available in Philadelphia, West Chester, Phoenixville, and Chester, PA. Knowing which services are covered, and exploring our additional services, helps families budget and plan for any gaps. It's important to note that while Medicare covers skilled medical care, non-medical personal care services, which are crucial for daily living, are typically not covered and represent the largest out-of-pocket expense for families, often ranging from $20-$35 per hour depending on location and service intensity.
Post‑hospital support at home combines practical care, careful medication oversight, therapy, and emotional support to help people recover more fully. When families understand the available services, financial options, and how technology can help, they can make clearer choices for safety and long-term well-being. For families seeking comprehensive guidance through the complexities of aging and care, our aging coach services can provide invaluable support. With the right plan and support, returning home becomes a step toward healing rather than a source of worry. To learn more about how we can support your family's recovery journey, please contact us today.
Frequently Asked Questions
What should I look for when choosing a caregiver for post-hospitalization support?
Look for caregivers with training and experience matched to your loved one’s needs — for example, medication management or mobility support. Good communication, patience, and references from other families matter. A caregiver who listens and follows the care plan will make the recovery smoother. The National Association for Home Care & Hospice recommends verifying a caregiver's certifications and background checks, as these are strong indicators of professional competence and trustworthiness.
How can technology improve post-hospitalization care at home?
Technology helps teams stay connected and monitor recovery. Telehealth visits, remote monitoring devices, and medication reminder tools make it easier to catch issues early and keep care coordinated between providers, caregivers, and family members. A recent survey by the American Telemedicine Association found that 85% of patients felt more connected to their care team and more confident in their recovery when using telehealth tools post-discharge.
What role does family involvement play in post-hospitalization recovery?
Family support is very important. Loved ones can help reinforce medication schedules, encourage therapy exercises, and provide emotional comfort. When families work with caregivers and clinicians, the care plan tends to be more consistent and effective. Studies show that strong family involvement can reduce readmission rates by an additional 10-15% when combined with professional home care, acting as a crucial layer of support.
How can I ensure my loved one adheres to their medication regimen?
Set a clear routine and use tools like pill organizers or reminder apps. Caregivers can provide daily checks and track side effects. Open conversations with clinicians about the purpose and timing of medicines also improve understanding and adherence. According to the Centers for Disease Control and Prevention (CDC), consistent medication adherence can reduce the risk of adverse health events by up to 60% for patients with chronic conditions.
What are the signs that a patient may need additional support after returning home?
Watch for trouble doing daily tasks, confusion about medications, worsening pain, shortness of breath, or changes in mood and behavior. If family caregivers feel overwhelmed, or if symptoms worsen, it’s time to arrange more professional support. The American Medical Association advises seeking immediate professional assessment if a patient experiences new or worsening symptoms such as fever, severe pain, or significant changes in mental status, as these can indicate serious complications.
How can emotional support be integrated into post-hospitalization care?
Emotional support can be built into care through regular companionship, encouraging activities, and checking in on mental health. If needed, involve counselors or therapists. Simple daily conversations and social engagement often make a big difference. The National Institute of Mental Health emphasizes that addressing emotional well-being is as crucial as physical recovery, noting that untreated depression can significantly impede physical healing and increase recovery time.


